Day 2 :
Keynote Forum
Istvan Berczi
University of Manitoba, Canada
Keynote: Initial studies on Neuroimmune Biology
Time : 09:30-09:55 AM

Biography:
István Berczi was born in Békés, Hungary. He graduated in 1962 in Budapest as Doctor of Veterinary Medicine, and was than research fellow in the Veterinary Medical Research Institute of the Hungarian Academy of Sciences (1962-67). He moved to Montreal as post-doctoral fellow of Selye (1967-68). Obtained PhD in Immunology (1972) and since 1991 he is Professor of the Department of Immunology at the Faculty of Medicine, University of Manitoba, Winnipeg, Canada. His main research field is the connections between hormonal regulation and immune regulation. He published 191 papers and book chapters, 8 books; 75 abstracts. Many of his discoveries (antibodies against endotoxins, tumor infiltrating lymphocytes, drug-antibody conjugates, bromocryptine, glandular Kallikrein) gained clinical applications.
Abstract:
The first paper on Neuroimmune Biology was published in 1978, describing that hypophisectomized (HYPX) rats are immune-deficient. Additional experiments revealed that Prolactin (PRL) and Growth hormone (GH) restore the immune competence of HYPX animals. Replacement doses were effective in reconstitution. Other pituitary hormones were inactive [1]. The antibody response and delayed type hypersensitivity to dinitro-chorobenzene of rats were inhibited by HYPX [2,3]. An autoimmune disease of rats, Adjuvant Arthritis was also inhibited by HYPX [4].
PRL and GH stimulated c-myc and DNA synthesis in the bone marrow [5]. The bone marrow was found to be pituitary dependent [5]. Eventually it was detected that the entire growth and lactogenic hormone family (PRL has 3 isomers, GH 3 isomers and Placental lactogens are a multitude of hormones). Placental lactogens regulate fetal development. Indeed this GLH axis is very powerful and support not only immune function but has a developmental role. The HPA axis is also heterogeneous so far 3 form of ACTH are known to exist [5].
We might ask why only Adaptive Immunity is regulated by such powerful mechanisms. Adaptive Immunity is clearly important. It provides antibodies and killer/regulatory T cells for immunity and inflammatory reactions. We observed that long surviving HYPX rats have residual prolactin in their blood. If this PRL is neutralized by antibodies the rats die within 6 weeks [5]. These animals have an intact innate immune system but this kind of immunity does not defend life, you need to have adaptive immunity for survival.
Keynote Forum
Michael V Ugrumov
Institute of Developmental Biology RAS, Russia
Keynote: Novel paradigm of the development of preclinical diagnosis of Parkinson’s disease
Time : 09:55-10:20

Biography:
M. Ugrumov graduated from Moscow University Medical School (USSR), obtained PhD at the Institute of Evolutionary Physiology and Biochemistry RAS (Leningrad, USSR) and Professorship in Anatomy and Physiology at Institute of Developmental Biology RAS and in Radiology and Pharmacology at State Medical University (Moscow, Russia). Ugrumov was elected as a full member of the Russian Academy of Sciences, European Academy of Science and Arts, Serbian Academy of Sciences and Arts, French National Academy of Pharmacy and nominated as a visiting Professor in Japan (Tokushima University Medical School), US (SUNY Upstate Medical University, Syracuse, NY), France (University P. et M. Curie, Paris, University of Tours) and Germany (University of Ulm). Ugrumov is a chair of the scientific council on Neuroscience and Neurotechnologies at the Ministry of Education and Science of RF President of the Russian Society for Neurochemistry. Main interests: Developmental neurobiology and neuroendocrinology, Neurodegenerative diseases.
Abstract:
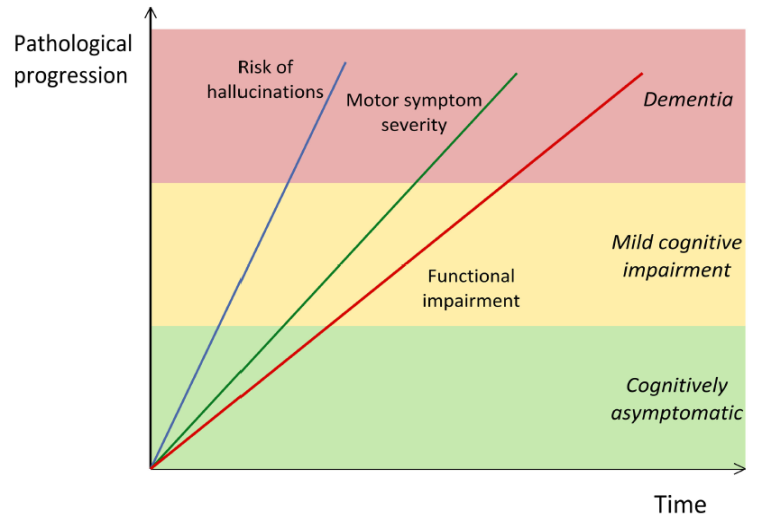
Motor symptoms first appear at Parkinson's disease (PD) many years after the onset of the degradation of the nigrostriatal system, at a loss of most dopaminergic (DA-ergic) neurons and depletion of neuroplasticity, which explains low efficiency of current therapy. Therefore, the development of the diagnostics of PD at the preclinical stage is of the highest priority. It is mainly based on a search for biomarkers as a change in the composition of plasma and expression of specific genes and phenotype of blood cells in untreated patients at the early clinical stage although there is no guarantee that biomarkers, found at the clinical stage are also characteristic of preclinical stage. That is why, in addition to patients, we searched for biomarkers in the blood in MPTP-treated mice at the early symptomatic stage and presymptomatic stage of parkinsonism. According to our data, the concentration of some markers in plasma, e.g., L-DOPA, were modified in the same way in PD patients and mice at both stages of parkinsonism. The concentration of others, e.g., DOPAC differed at the presymptomatic stage in mice from those in mice at the symptomatic stage and patients. Apparently the former markers are more reliable than the latter. Moreover, in experimental models, we developed a new approach to preclinical diagnosis of PD by using a pharmacological provocation test (reversible inhibitor of dopamine synthesis), which induces a short-term increase in failure of the nigrostriatal system and the appearance of motor disorders. Development of preclinical diagnostics of PD basing on the search for biomarkers in the blood in untreated PD patients and experimental models and the use of a provocative test would allow to use neuroprotective pharmacotherapy for slowing down neurodegeneration and thereby prolongation of a asymptomatic period.
Keynote Forum
Ni Hong
Soochow University , China
Keynote: Molecular mechanism and intervention studies of regenerative mossy fiber sprouting in hippocampus following developmental seizures
Time : 10:20-11:05

Biography:
Ni Hong, Ph.D., works in the Children’s Hospital of Soochow University (China) as Pediatric Neurologist with main interest in Pediatric neurological rehabilitation, cerebral palsy and epilepsy since 1995. He is a professor and the lead of the Department of Brain Science, Institute of Pediatric Clinical Research, Soochow University. He has published more than 60 journal articles mainly with developmental neuroscience. He is now a member of the Chinese society of microcirculation council.
Abstract:
Developmental seizure-induced brain damage can cause serious neurological sequelae. Denervation and regenerative mossy fiber (MF) sprouting in the hippocampal dentate gyrus and CA3 subfields are the main neuroanatomical bases. We used several developmental epilepsy animal models to study the mechanism of seizure-induced mossy fiber sprouting and intervention strategy. We found that recurrent prolonged developmental seizures induced by penicillin or inhalant flurothyl can cause long-term cognitive deficit and hippocampal regenerative sprouting in adulthood, which is in parallel with long-term significantly up- or down-regulated expression of zinc transporters (ZnT1,ZnT3,ZIP6), plasma membrane damage associated-lipid metabolism molecules (PRGs, Cyp46a1, cPLA2, ACAT1, nSMase, Kcnj11, Lepr, Drd2, Mc4r, Apoa1, Oprk1, Pdk4, ApoE) and autophagy markers (beclin-1, LC3, p62, cathepsin E) in the hippocampus. Moreover,there were significantly correlation among autophagic, Zn transporter signaling and lipid metabolism molecules. Ketogenic diet, plasma membrane oxidant injury protectant melatonin, lipid metabolism regulating molecule leptin, autophagy inhibitors (3-MA, CBI, E-64d), as well as early physical exercise were able to restore the abnormal expressions to normalize and alleviate the aberrant hippocampal MF sprouting, neurobehavioral and cognitive changes, which may be achieved through cPLA2/drp1/autophygy pathway, and by regulating the expression of Zinc/CaMK II signaling. Our study will be helpful for exploring the target genes of axonal regeneration following developing seizures from a new point of view and will contribute the efforts for making proper early intervention, as well.
Keynote Forum
M Cohen-Armon
Tel-Aviv University, Israel
Keynote: PARP1 dependent long-term memory acquisition
Time : 10:20-11:05

Biography:
Education in theTechnion, Israel, B.Sc. Chemistry (cum laude) and D.Sc., Biophysics & Electrophysiology. Academic position at the Tel-Aviv University Life Science, Neurobiochemistry, and 1992-present: Faculty of Medicine, Dept. of Physiology and Pharmacology. On 2001, she was a visiting researcher in Columbia University, New York, lab of Learning and Memory, in collaboration with Late Prof. James Schwartz. Prof Cohen-Armon is an academic editor in PLOS ONE and Am. J. of Alzheimer's Disease & Other Dementias, She is the recipient of numerous professional awards including HFSP. She authors several high impact papers. Her discovery on the voltage dependence of GPCR affinity for their agonists (reported in PNAS and J Biol Chem) developed into a new research field. On 2004 Dr Cohen-Armon and Prof Schwartz first reported on a mechanism in the chromatin that is required for long-term memory acquisition during learning. Their finding was reported in Science, and was accompanied by Press release in USA and Israel. Their discovery lead to the disclosure of epigenetic mechanisms underlying addiction. Through 2000-2007 Dr Cohen-Armon identified the role of the chromatin-bound protein PARP1 in signal transduction mechanisms evoking gene expression in response to excitatory signals (reported in J Cell Biol, J Neurosci, Mol Cell, TIPS). The implication of this molecular mechanism in synaptic plasticity and long-term memory is the main topic of her current research. On 2009 Dr Cohen-Armon discovered that human solid cancer cells are exclusively eradicated by a small molecule, the phenanthridine PJ34, which protects human normal cells from apoptotic cell death. She identified the exclusive death mechanism activated by this molecule in human cancer cells during mitosis. Her finding was accompanied by a word wide press release, and was patented. At present, her applied research on PJ34 is supported by Novartis.
Abstract:
Unexpectedly, a post-translational modification of DNA-binding proteins, initiating the cell response to single-strand DNA damage, is also required for long-term memory acquisition in a variety of learning paradigms. Our findings disclose a molecular mechanism based on PARP1-Erk2 synergism, which may underlie this phenomenon. A stimulation induced PARP1 binding to phosphorylated Erk2 in the chromatin of cerebral neurons caused Erk-induced PARP1 activation, rendering transcription factors and promoters of immediate early genes (IEG) accessible to PARP1-bound phosphorylated Erk2. PARP1 inhibition, silencing, or genetic deletion abrogated stimulation-induced Erk-recruitment to IEG promoters, IEG expression and LTP generation in hippocampal CA3-CA1-connections. Moreover, a predominant binding of PARP1 to single-strand DNA breaks, occluding its Erk binding sites, suppressed IEG expression and prevented the generation of LTP. These findings suggest that Erk-induced PARP1 activation mediates IEG expression implicated in synaptic plasticity and in long-term memory acquisition which deteriorates in senescence when aged cerebral neurons accumulate DNA single-strand breaks. These findings may be also implicated in a PARP1 dependent mechanism associated with reward-related memory retrieval
- Track 1: Neuroimmunology and Neuroinflammation | Track 6: Neurochemical Transmission | Alzheimer’s Disease and Dementia | Track 11: Parkinson’s Disease
Location: Hilton Garden Inn Milan North Via Lucio Giunio Columella, 36, 20128 Milano, Italy
Session Introduction
Christina Francisca Vogelaar
Johannes Gutenberg University Mainz, Germany
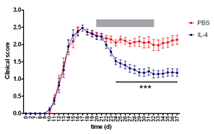
Title: Fast direct neuronal signaling via the IL-4 receptor reverses disease severity in progressive neuroinflammation

Biography:
Christina Francisca Vogelaar has her expertise in nerve regeneration. Her research focusses on the molecular mechanisms of peripheral and central axon regeneration and the treatment of traumatic and neuroinflammatory axon injury. She worked on sciatic nerve regeneration, on axonal RNA localization, and on spinal cord injury. In Mainz (Germany), her group works on ribosome transport and transfer in axons. She recently joined the lab of Frauke Zipp (Mainz, Germany) to investigate axon repair in neuroinflammation.
Abstract:
Marina Farinelli
Clinical Psychology Service “CASA DI CURA VILLA BELLOMBRA†rehabilitation hospital - Consorzio Colibrì - Bologna, Italy
Title: The Impact of Brain Lesions On Basic Emotions And Emotion Regulation In Stroke Survivors

Biography:
Marina Farinelli is MD, specialist in clinical psychology, psychotherapist and psychosomatic specialist (ICPM). Her main fields of interest for research and clinical practice are the psychosomatic approach and neuroscience. She taught at Bologna and Chieti Universities (Italy).
Working with neurological patients at Villa Bellombra Rehabilitation Hospital (Bologna) since 1996, she established and currently coordinates a Clinical Psychology Service to support patients and their caregivers, integrate the multi-professional team and carry out researches. Since 2009 she has been coordinating the research project devoted to stroke patients entitled “The impact of brain lesion on internalization/externalization processes: a neuropsychodynamic study” carried out in collaboration with the Neuroradiological Unit (IRCCS) of Bellaria Hospital of Bologna, the Dept. of Psychology of Bologna University and the Institute of Mental Health University of Ottawa. The clinical and research experiences and findings have been presented at numerous national and international congresses and published on scientific journals.
Abstract:
Statement of the problem: Panksepp (1998) first proposed an “affective neuroscience” approach to explore foundations of human and animal emotions in connection with specific subcortical brain systems which underlie the self (core Self) and the self-referential processing. In particular, four basic emotional systems (SEEKING, ANGER, FEAR and LUST) were identified having evolutionally deep reptilian roots and three (CARING, SADNESS and PLAY) reflect more uniquely mammalian adaptations. The Affective Neuroscience Personality Scales (ANPS) have been developed to evaluate these emotional, personality tendencies in humans. The alterations of basic emotions after brain injury according to Panksepp’s theory remain understudied. The aim of this presentation is to illustrate the outcomes of recent researches that studied basic emotions and emotion regulation in stroke survivors and their implication for pharmacological treatments and rehabilitation in clinical practice. Methodology: A sample group of stroke patients and a control group of orthopedic patients both hospitalized and in post-acute phase were evaluated by two self-report questionnaires: ANPS and HADS (Hospital Anxiety and Depression Scales) taking into account the location of brain damage. Findings: Stroke patients showed a statistically significant lower scores in ANPS-SEEKING and higher scores in depression by HADS in comparison with the control group. Moreover, further alterations in basic emotion systems in comparison to the control group were found, highlighting a specific pattern of emotion regulation. The involvement of anterior subcortical-cortical midline-structures was evident. Conclusions and significance: The specific changes and alterations of basic emotions and dispositions towards the external environment in relation to peculiar brain damage in stroke entail tailored stimulations and modulations of physiotherapeutic and pharmacological treatments during the rehabilitation process. Furthermore a tailored psychotherapeutic intervention often needs to support patients and their caregivers; the involvement of caregivers is necessary due to their role in emotion regulation in daily life.

Biography:
Varghese received his PhD from the Department of Medicinal Chemistry, University of Minnesota in 1985. He a postdoctoral fellowship in Professor Josef Fried’s lab in the Department of Chemistry, University of Chicago and a second postdoctoral fellowship in Professor Carl Djerassi’s lab in the Department of Chemistry at Stanford University. He worked with Athena Neurosciences/Elan Pharmaceuticals as a senior member of their Discovery team for 18 years. He then joined the Buck Institute for Research on Aging where he was Director of Alzheimer’s Drug Discovery Network. He started the Drug Discovery Lab at UCLA in 2015.
Abstract:
Apolipoprotein ε4 (ApoE4) is a major genetic risk factor for sporadic, late-onset Alzheimer’s disease (AD). One protein target that is affected in the presence of ApoE4 is the major longevity determinant and NAD-dependent deacetylase sirtuin-1 (SirT1), which we showed to be decreased in the presence of ApoE4 (Theendakara, PNAS 2013). Recent reports also show that SirT1 levels are shown to be decreased in serum of AD patients (Kumar, PLoS One 2013). Through screening we have identified a brain-penetrant small molecule, A03, that increased the neuroprotective SirT1 protein levels in ApoE4-transfected cells, and we have recently tested its efficacy in vivo in a ApoE4 mouse model for AD. The preliminary results show that A03 treatment can increase in SirT1 levels in the mouse brain thus providing initial proof-of-concept for developing this drug candidate as a ApoE4-targeted therapeutic for AD. We are in the process of designing and synthesizing analogs of A03, and studying their effects on both the neuroprotective SirT1 and neurotoxic protein sirtuin-2 (SirT2) in ApoE4-transfected cells. In addition, we have also initiated high throughput screening (HTS) of the UCLA compound library to identify new ‘hits’ that increase SirT1 in the presence of ApoE4. Our data thus reveal a novel mechanism for developing targeted therapeutics for this major known risk factor for AD. A03 is a promising lead candidate that increases brain SirT1 levels and could be developed as an ApoE4-targeted therapeutic for AD. Synthesis, testing, and screening of new ‘hit-analogs’ could yield additional candidates for development as potential therapeutics for Mild Cognitive Impairment (MCI) and/or AD. The research is supported by funding from NIH (R01AG051386) and the UCLA Easton Center for AD Research.
Alireza Rezayi
Shahid Beheshti University of Medical Sciences, Iran
Title: Intravenous Immunoglobulins for children Refractory Epilepsy

Biography:
Rezayi A.R has expertise in child neurology and he is working on rare disease such as neurometabolic and referactory epilepsy in thirthiary center of child neurology center(mofid children hospital and loghman hakim hospital) in Tehran, Iran.He is publicated several article in field of child neurology and he is faculty member of shahid beheshti university of medical sciences and interested in education of child neurology fellow and pediatric residents and medical students.He was certificated in Iranian child neurology national board in septamber2011 and he is membership in several international child neurology society such as ICNA(international child neurology association), AOCNA (asian and oceanian child neurology association),EPSN(European Paediatric Neurology Society) and Iranian child neurology association.
Abstract:
Statement of the Problem :This study was conducted to investigate the efficacy of intravenous immunoglobulin for drug-resistant seizures in children reffered to pediatric neurology clinic .
Methodology & Theoretical Orientation:A retrospective review of all children in loghman hakim hospital neurology clinic from 2012 to 2015, inclusive, with intractable epilepsy who were treated with intravenous immunoglobulin for a minimum of 3 cycles was performed. Data collected included seizure frequency, seizure and epilepsy syndrome type, propable etiology for the seizures, and. Response to intravenous immunoglobulin was defined as “positive” if either seizure freedom or ≥50% reduction of seizures was achieved.
Findings:fourteen children (8 m -12 years old) were included in the study. Treatment with intravenous immunoglobulin, the following outcomes were noted: Three were seizure-free, four had 90% reduction, two had 50% reduction,three had 30 % reduction and two had any responsivness. A total of 9 (64%) patients had a positive clinical response to IVIG treatment from baseline. Five patients (36%) were not responsive. No relationship of responsiveness to intravenous immunoglobulin with regard to age, gender, or epilepsy syndrome was detected.
Conclusion & Significance:Our study and others suggest that intravenous immunoglobulin can used in the treatment of children with drug-resistant epilepsies with potentially high efficacy and low side effect. This treatment was able to reduce multiple seizure types in a variety of epilepsy etiologies, including those of unknown cause or even inborn error of metabolism.
Eunji Cheong
Yonsei University, South Korea
Title: Thalamocortical circuit in sleep control: the thalamic mGluR1-PLCï¢4 pathway is critical in sleep architecture

Biography:
Eunji Cheong and her research group have expertise in studying electrophysiological properties of neurons from ion channel level to brain circuit level. Her lab has studied the thalamocortical circuit in controlling the vigilance state of brain such as sleep state control and pathological impairment of consciousness in mice model for many years. She also worked on studying the ion channels and synaptic transmission which control the excitability of thalamocortcial neurons. She has published over 30 research papers in prestigious journals during the last 5 years
Abstract:
The transition from wakefulness to a nonrapid eye movement (NREM) sleep state at the onset of sleep involves a transition from low-voltage, high-frequency irregular electroencephalography (EEG) waveforms to large-amplitude, low-frequency EEG waveforms accompanying synchronized oscillatory activity in the thalamocortical circuit. The thalamocortical circuit consists of reciprocal connections between the thalamus and cortex. The cortex sends strong excitatory feedback to the thalamus, however the function of which is unclear. Here we investigated the role of the corticothalamic inputs onto thalamcortical (TC) neurons via metabotropic glutamate receptor 1 (mGluR1) pathway in sleep control. The mGluR1 in TC neurons is linked to phospholipase C b4 (PLCb4) pathway. In PLCβ4-/- mice, the transition from wakefulness to the NREM sleep state was stimulated, and the NREM sleep state was stabilized, which resulted in increased NREM sleep. The power density of delta (δ) waves increased in parallel with the increased NREM sleep. These sleep phenotypes in PLCβ4-/- were consistent in TC-restricted PLCβ4 knockdown mice. Moreover, in vitro intrathalamic oscillations were greatly enhanced in the PLCβ4-/- slices. The results of our study showed that top-down control of thalamocortical circuit was critical in controlling sleep architecture.
Mariya Hristova
University College London, UK
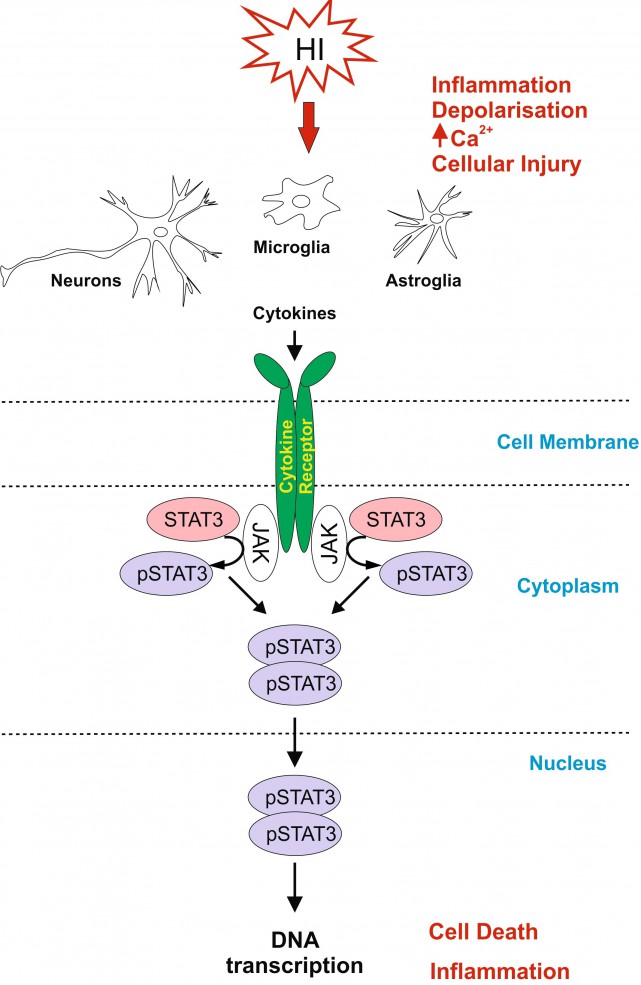
Title: Inhibition of Signal Transducer and Activator of Transcription 3 (STAT3) reduces neonatal hypoxic-ischemic brain damage

Biography:
Dr Mariya Hristova is Senior Research Associate and leads the Perinatal Brain Repair Group at the Institute for Women’s Health, University College London. She has very strong expertise in neuroimmunology and in the hypoxia-ischaemia model, therapeutic hypothermia and brain analysis investigating the role of post-translational modifications, transcription factors (STAT3), cytokines (TNFa) and pH changes following neonatal hypoxia-ischaemia. She has been an essential part of the team studying the combination of xenon and therapeutic hypothermia, and melatonin and therapeutic hypothermia in a neonatal piglet model of transient birth asphyxia.
Abstract:
Neonatal hypoxic-ischaemic encephalopathy (HIE) is a leading cause of neonatal mortality and morbidity, affecting 1-3 per 1000 live-births in developed countries with rates about 5-10 times higher in low-income setting. About 40% of the affected children die in the neonatal period and further 30% develop life-long disabilities such as cerebral palsy, epilepsy and mental retardation. Therapeutic hypothermia is the only clinically approved care for moderate to severe neonatal hypoxic-ischaemic (HI) brain injury, however it reduces death and disability only by 11% with about 40% of the treated infants still developing neurological incapacities. For hypothermia to be effective, 7-8 infants need to be treated for one to benefit from the treatment. Therefore it is necessary to develop simple, safe and effective supplementary therapies to add to the current therapeutic strategy in infants with HIE.
Signal Transducer and Activator of Transcription 3 (STAT3) is strongly up-regulated by HI in the immature brain. To investigate the association of STAT3 up-regulation with HI-brain damage, and whether phosphorylated STAT3 originating from different cell types has a different role in promoting HI-damage, we subjected postnatal day seven mice to unilateral carotid artery ligation followed by 60min hypoxia. Neuron-specific STAT3-deletion reduced microglial and astroglial activation, cell death and tissue loss in all brain regions. Astroglial STAT3-deletion also reduced microglial activation, cell death and tissue loss, although not as much as neuronal deletion. Systemic STAT3-inhibition with JAK2-inhibitor WP1066 only moderately reduced microglial and astroglial activation, but in a pattern similar to the one observed with the cell-specific deletions. Our results suggest that STAT3 is an important factor in neonatal HI-brain damage and its removal in neurons or astrocytes, and, to some extent, systemic inhibition reduces inflammation and tissue loss. Overall, the protective effects of STAT3 inhibition make it a potential target for a therapeutic strategy in neonatal HI.
Joel B Schachter
Merck Research Laboratories, USA
Title: Can Tau Pathobiology be Pheno-copied in a Cellular Expression Model?

Biography:
Joel Schachter is currently a Principal Scientist in the Movement Disorders and Translation Group at Merck. Dr Schachter joined Merck in 2009 as Director of Neurology and has held several positions there including head of External Discovery and Preclinical Sciences for Neuroscience (XDPS) and Franchise Collaboration Lead for Neuroscience. In his role within XDPS, he was involved in building effective collaborations with external partners and in execution of preclinical drug discovery programs in the areas of Alzheimer's Disease, Parkinson's Disease, Schizophrenia, and pain/migraine. As Franchise Collaboration Lead, he developed collaborative basic research efforts with academic partners. Prior to his work at Merck, Dr Schachter spent 12 years at Pfizer as a member of the Molecular Sciences Department and the Neurology group where he led project teams for several Alzheimer’s Disease-related drug discovery programs including GSK3, Gamma modulators, and Tau New Targets
Abstract:
Tau hyperphosphorylation and formation of insoluble tau deposits are principal aspects of the neurofibrillary pathology associated with Alzheimer’s disease (AD) and other neurodegenerative Tauopathies. Despite a histology-based focus on insoluble filamentous tau pathology, small soluble tau oligomers have recently been implicated in the promotion of neurodegenerative activities and are now widely viewed as central participants in disease-related neurodegeneration. The factors that initiate the aberrant post-translational processing of tau and the generation of toxic tau oligomers are not well defined, but hyperphosphorylation has been implicated to play a critical role in tau aggregation. We have generated a cellular model in which full length human tau is expressed as a dimer-like structure that we refer to as “tandem repeat tau” (TRT). Cellular expression of TRT results in rapid hyperphosphorylation of the protein at disease-relevant epitopes. The rapid hyperphosphorylation is followed by a slower formation of high molecular weight tau oligomers that are stable to detergent extraction and gel filtration. TRT displays proteolytic processing with multiple cleavage products that are not observed for the monomeric version of tau. Cells expressing TRT show increased propensity for caspase activation and an activation of the unfolded protein response, suggesting that TRT expression initiates a cascade of pathological cellular responses that compromise cellular viability. Given multiple observations of similar post-translational processing of TRT in this model, compared to tau pathology in brains of patients with AD and other neurodegenerative Tauopathies, we suggest that this model may be useful for delineating cell biology associated with Tauopathy, as well as providing a model system for testing potential therapeutic agents.
Aruna Sharma
Uppsala University, Sweden
Title: Nanodelivery of cerebrolysin induces neuroprotection in Parkinson’s disease

Biography:
Aruna Sharma, MD is currently Secretary of Research at Uppsala University Hospital, Uppsala University, Sweden. She obtained her Bachelor of Science in 1971 and trained in Indian Medicine up to 1977 and engaged in medical research from 1978 to 1986 in India on hyperthermia induced brain dysfunction in the lab of Hari Sharma and Prasanta Kumar Dey under University Grants Commission and Indian Council of Medical Research Programs. She is a qualified experimental Neurpathologist and received her training at Karl Marx University Leipzig, Institute of Neurobiology (1987-1988); Semmelweis University Medical School, Department of Human Morphology and Developmental Biology, Budapest, Hungary (1988-1989), Free University Berlin, Germany (1989-1991) and Neuropathology Institute Uppsala (1992-1995). Dr Sharma is member of various Distinguished American Organizations and elected to receive the prestigious award “Women of the Years Representing Sweden Award 2009” for her outstanding contributions towards society by American Biographical Research Institute, USA; and “Best Professional Business Women Award 2010” For Setting Standard to Motivate, Excel and Inspire Others, Raleigh, North Carolina, USA. She has published over 50 original research papers in Reputed Neuroscience Journals and is currently Acquisition Editor of American Journal of Neuroproetction and Neuroregenartion.
Abstract:
Parkinson’s disease (PD) affects over 80 thousand Americans every year for which no suitable therapy is available till date. PD induces severe disability in victims and so far no suitable strategies have been developed resulting an urgent need to explore novel therapeutic strategies to treat PD for the benefit of the mankind. Recently, nanodrug delivery of therapeutic compounds has been shown to induce superior neuroprotective effects than the parent compounds in central nervous system (CNS) diseases.
There are evidences that increased oxidative stress and neurotoxic elements in the CSF and in the brain appears to be responsible for PD pathology and decline in cognitive and motor functions. Recent research suggests that increased alpha-synuclein (ï¡-synuclein, ASNC) in the CSF and in several brain areas together with oxidative stress correlates well with the brain pathology and cognitive decline in human cases of PD. Thus, a possibility exists that drugs that are capable to reduce the levels of oxidants and/or ASNC could be useful for novel therapeutic tools in PD.
Previous reports from our laboratory showed that intraperitoneal injections of 1-metyl-4-fenyl-1,2,3,6-tetrahydropyridin (MPTP, 20 mg/kg) daily within 2-h intervals for 5 days in mice induce PD like symptoms on the 8th day. This model is well-characterized biochemically, histologically and functionally for PD like symptoms. Thus, marked decrease in the number of tyrosine hydroxylase (TH) positive cells in the Substantia Nigra Pars Compacta (SNpc) and striatum (STr) as well as decrease in dopamine (DA) and its metabolites 3,4-Dihydroxyphenylacetic acid (DOPAC) and homovanillic acid (HVA) with marked behavioral dysfunctions e.g., Rota-Rod performances, walking on an inclined mesh grid and gait deficits was seen on the 8th day.
Cerebrolysin (CBL) is a well-balanced composition of several neurotrophic factors and active peptide fragments. Thus, this multimodal drug may have an added value on therapeutic strategies in PD. In present investigations we examined timed release of CBL using titanate nanospheres (TiNS) in treating PD in our mouse model. In this investigation, timed release of CBL using titanate nanospheres (TiNS) treatment results in significant neuroprotection and behavioral improvements. Thus, it would be interesting to examine whether this model of PD is also associated with increased ASNC and free radical nitric oxide in the CSF and brain areas of mice and cerebrolysin treatment could modulate these elements in our model.
ASNC was measures using commercial ELISA kit in the CSF and in brain whereas neuronal nitric oxide synthase (nNOS) was examined using immunohistochemistry on paraffin sections. Our results showed a significant increase in ASNC by 2- to 4-fold in the CSF and in various brain areas from normal control group (control: SNpc 1.78±0.08 ng/mg, STr 6.34±0.21 ng/mg, frontal cortex 8.24±0.32 ng/mg; CSF 1.21±0.07 pg/ml). In these brain areas nNOS expression was also increased by 4- to 8-fold as compared to control group. Nanodelivery of cerebrolysin (3 ml/kg, i.v. 2 days after MPTP for 5 days) significantly reduced ASNC levels in the CSF and in all the brain areas examined. In the treated PD mice downregulation of nNOS was also seen in the above brain regions. These results are the first to show that nanodelivery of cerebrolysin induces neuroprotection in PD by reducing ASNC and nNOS expression. However, further research is needed to explore TiNS in clinical situations, a feature that requires additional investigations.
Ying-Chieh Tsai
National Yang-Ming University, Taiwan
Title: Psychobiotic PS128 rescued motor deficits in MPTP-induced mice model

Biography:
Abstract:
Parkinson’s disease (PD) is a common neurodegeneration disease caused by dopaminergic neuron degeneration in brain. The dopamine signaling collapsed and resulted in motor deficits like shaking, difficulty with walking and gait in PD patients. Recent studies have revealed that gut microbiota influence neurodevelopment, modulate behavior, and contribute to neurological disorders through microbiome-gut-brain axis (MGBA). Certain probiotics strain, or “psychobiotics”, even showed unique psychotropic effects in many animal studies and clinical trials. Lately, we found a special psychobiotic Lactobacillus plantarum PS128 which improved dopamine transmission in brain specific regions and modulated behaviors in different mice models, raising the possibility that that PS128 might show beneficial effect on host’s CNS dopamine system through MGBA. In this study, we used 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) to establish a PD-like mice model to investigate whether PS128 also show neuroprotective effect on host’s CNS dopamine system. PS128 was oral administered to mice for 4 weeks before 5-day MPTP injection. We found PS128 significantly improved the pole test, narrow beam test, and rotarod test performance, indicating that it rescued MPTP-induced motor deficits. Further brain tissue analyses showed that PS128 prevented MPTP-induced dopaminergic neuron loss in substantia nigra and rescued dopamine & noradrenaline total level in striatum. In conclusion, PS128 could prevent MPTP-induced motor deficits, dopaminergic neuron loss, and neurotransmitter signaling collapse. PS128 might show neuroprotective potential on host’s CNS dopamine system leading to clinical application for treating and preventing PD or other dopamine-related neuropsychiatric disorders.
Image
Psychobiotic PS128: start with mental health, step forward to brain health
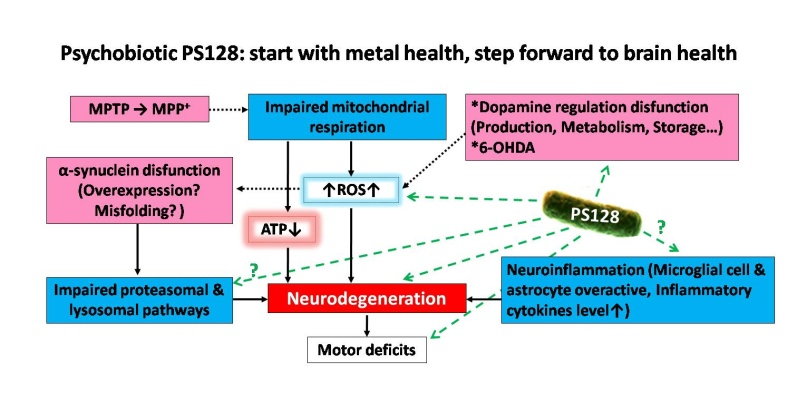
Figure 1: The proposed pathways of Parkinson’s disease (PD) & PD-like animal models and the possible mechanisms of PS128 neuroprotective effects on host’s CNS dopamine system.
Elizabeth K Barber
Barber Innovations LLC, USA
Title: Therapeutic Strategies for the Parkinson's Patient with Alzheimer's Changes: The Benefits of Art, Structure and Nutrition

Biography:
Elizabeth Barber has a long interest in integrative medicine, extensive experience as a Parkinson's Disease (PD) care manager as well as graduate work in signal transduction. She completed her BA with Honors, receiving the Robie Medal for outstanding graduate then Rotary Ambassadorial Scholar. At Harvard, she completed a master's in Biology, co-authoring several publications. Her doctorate at Oxford University on CD33 and CD34 in Biochemistry included neuromuscular disease. She became a trial lawyer/advocate at in London which she then applied to organize the many care, administrative and advocacy issues of PD from 2003 to 2015. She was invited to join the American Academy of Neurology in 2005 which selected her as a Palatucci Leadership Forum Advocate. She combined her knowledge of Art, interior design and science to develop an integrative care plan, serendipitously discovering a PD treatment, starting Barber Innovations LLC to develop her research while managing patient care.
Abstract:
Statement of the Problem: Parkinson's Disease (PD) has traditionally been treated mainly with drugs upon presentation of a tremor, stiffness or weakness by the patient which usually progresses to include "Alzheimer's Changes" or PD dementia when the patient is often transferred to a nursing facility. Epigenetics and nutragenomics show that we can improve our health through diet and lifestyle changes, as certain pesticides are known to cause PD.1 Staying in the home is generally less expensive than a nursing home with better health outcomes. Methodology and Theoretical Orientation: This case study presents the long-term therapeutic benefits of a preventive strategy creating a positive and safe neurological environment. A combination of therapeutic art,2 design, structured meals, medication, supplements, exercise, reducing environmental and food toxins was integrated to develop a workable strategy for providers and families to manage the disease. Following a fall and hospitalization, a stepwise program was developed and implemented in the home using the patient's preferences and research to allow for a smooth transition from rehabilitation into a neurologically therapeutic environment integrating art and healing interior design.3 The environment was made safer, a system of medication and meal administration highlighting neurologic and intestinal health was implemented and a caregiver instruction system was established. Certain nutritional supplements4-5 and regular exercise were integral treatment arms. A team approach to care was emphasized, including family members and providers. Findings: The combination of therapeutic approaches and strategies was found to be particularly helpful and significantly increased the patient's lifespan as well as lowering the home stress level. The therapeutic strategies were put into a teaching tool, so that new caregivers and family members could be taught the program and prepare for disease progression. Conclusion & Significance: The checklist of strategies used at different stages of the disease will aid providers, patients and their families in coping with and ameliorating PD difficulties.
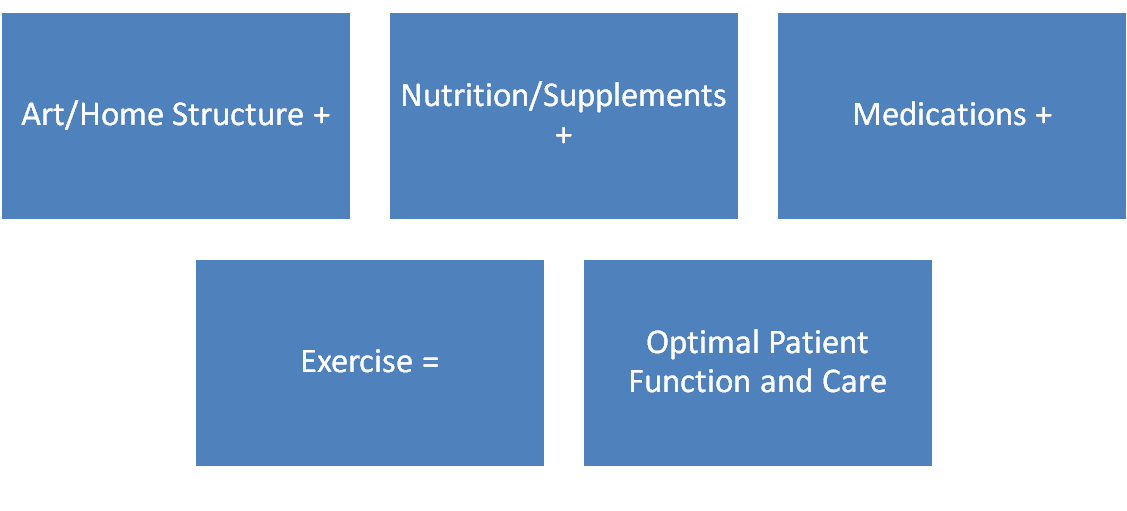
Figure 1. Integrated Aspects of Parkinson's Disease Care. An effective care plan includes Nature Art, a Structured Home Environment, Targeted Nutrition and Supplements, Scheduled Medication and Targeted exercise for optimal patient function and care.
Michel CYR
University of Trois-Rivieres, Canada
Title: Oral treatment with sphingosine-1-phosphate receptors modulator prevents Parkinson symptoms concomitantly to reduced brain inflammation in MPTP mouse models

Biography:
Michel CYR is a PhD holder in Pharmacy from Laval University in Canada and a Post-Doctoral Trainee in Cellular Biology at Duke University in the USA. He is currently a Full Professor at the Medical Biology Department at the University of Trois-Rivieres. As the Director of the Canada Research Chair in Molecular Neuropharmacology, he is leading the effort to understand the molecules in the brain that are responsible for learning and executing motor actions. He is also investigating the molecular bases for movement disorders such as Parkinson disease and makes it possible to better target and develop new treatments.
Abstract:
Here we explore the efficacy of an oral treatment with fingolimod (FTY720), a selective sphingosine-1-phosphate receptors modulator, to prevent MPTP induced nigrostriatal loss and motor deficits in mice. In addition, potential molecular mechanisms have been assessed. Sphingosine-1-phosphate is a potent bioactive lipid mediator that acts as a natural ligand upon binding to five different receptors that are located in astrocytes, oligodendrocytes, microglial and neuronal cells. Modulation of these receptors has been shown to provide neuroprotection in multiple sclerosis and in mouse model of Alzheimer’s disease. Whether the selective sphingosine-1-phosphate receptors modulator FTY720 exhibits neuroprotection in Parkinson’s disease is unclear. Adult male mice were disseminated into four independent groups: vehicle (saline), FTY720, MPTP/vehicle and MPTP/FTY720. Chronic oral FTY720 (1 mg/kg) administrations began two days before the MPTP (30 mg/kg, i.p., 5 days) treatments. Motor behavioral tests and Western blot analyses on striatum tissues were assessed on these mice. We revealed diminutions of ~50% in the levels of tyrosine hydroxylase and dopamine transporter proteins in the striatum of MPTP mice. At the behavioral level, these mice exhibited motor deficits at the Pole and Beam tests. Interestingly, FTY720 oral treatment has the capacity to prevent these known detrimental signs associated to MPTP treatment. Further study has revealed that while striatal levels of phosphorylated extracellular signal-regulated kinases and S1PR subtype 1 were unaffected, tumor necrosis factor-alpha and glial fibrillary acidic protein levels were robustly increased in MPTP-treated mice, an outcome that was totally prevented by FTY720 treatments. Notably, FTY720 treatments was also able to prevent the reduction of brain-derived neurotrophic factor levels observed in the striatum of mice treated with MPTP. Our findings propose that oral FTY720 treatments prevent the damaging effects of MPTP on striatal dopamine terminals and motor behaviors. The mechanism of action may involve inhibition of inflammatory pathways and the modulation of brain-derived neurotrophic factor synthesis. This study is providing novel evidence for the clinical utility of targeting S1PR in Parkinson’s disease therapy.
Safa Najmi Tabrizi
Tabriz University of Medical Science, Iran
Title: Addiction and Withdrawal of Dopamine Agonists Therapy for Parkinson’s disease

Biography:
Dr. Safa Najmi Tabrizi, Born in 1972 in Tabriz, Iran; is an Assistant Professor of Neurology in Tabriz University of Medical Science in Iran. After Graduation in Neurology as a board certi,ied, he trained in Parkinson’s disease and Dementia in Istanbul medical University. Also, he was a research fellow in Washington University at Saint Louis and Saint Louis University in USA in 1ield of Dementia and Neurodegenerative disorders. He has had many lectures as an invited speaker in several international meetings and congresses. Safa Najmi has many articles and publications at different scienti4ic journals.
Abstract:
Hossein Ali Ebrahimi
Kerman University of Medical Sciences, Iran
Title: Multiple sclerosis and mines

Biography:
I am Hossein Ali Ebrahimi Meimand, Professor of neurology in neurology department of Kerman University of medical Sciences. I was born in Shahrbabak city of Kerman province of Iran at 15/3/1954. The my interests in neurology are epilepsy and multiple sclerosis, I have many articles in national and international indexed journals, more than 80 articles and near 100 abstracts in medical congresses, and I wrote a book about guideline of epilepsy management (Persian language). At know I am head of Neurology Research Center in Kerman University of Medical sciences, Kerman, Iran.
Abstract:
Multiple sclerosis (MS) is the most common inflammatory-demyelinating disease of the central nervous system.
Our knowledge about its pathogenesis is still incomplete and etiology remains unknown, early observations showed that the prevalence of MS is variable among geographic areas. One of the most geographic differences among areas of the world is mines existence. Also, available articles provide evidences of the effect of metals in MS pathogenesis. For example, iron, selenium, zinc, cooper.
Kerman province is a vast region with an area of 714,181 square kilometers located in southeastern Iran (latitude 30° north). Epidemiology of MS in different area of Kerman province are varied. Of course we observed an latitudes differences in different areas of Kerman province.
A cross-sectional study was conducted on MS patients in Kerman province in 2012. The details of the patients including age, sex, age at the onset of disorder and disease duration were collected from documents of MS centers of all cities. Diagnosis was confirmed according to the revised Mc-Donald criteria.
The climate varies in different parts of Kerman province. The rate of MS patients in Sirjan city with mines of iron is near 32, Rafsanjan city with some cooper mines is 27,and in Zarand city with a lot of coal mines is 27, these cities are dry and with an average temperature range of 16–20°C. The rate MS patients in Kahnuj city is near 2, Bam 17.5, and Jiroft, 14, these cities are warm and semi humid weather (average temperature of >20°C).
The mean prevalence of MS in mineral areas in Kerman province (Kahnoj, Sirjan, Zarand, Rafsanjan, Baft, Shahrbabak) was 23.01±10.78 and in non-mineral areas (Kerman, Bam, Jiroft) was 39.56±20.34 that show the higher prevalence of MS in non-mineral areas of Kerman province. A linear relationship between an increase in prevalence and low average temperature was observed. In the town of Shahrbabak which has cold weather, prevalence was low, which might be related to the presence a lot of copper mines in this area, because the ccooper is used in the synthesis of myelin.
Ola Ahmed Heikal
National Research Center, Egypt
Title: Rice bran, a Functional extract, new scientific evidences for potential health benefits in Alzheimer’s disease therapy

Biography:
Professor of analytical toxicology and head of department at The National Research Center (NRC) 2003, and professor in German university in Cairo (GUC) previously head of department of pharmacology & toxicology; faculty of pharmacy ( 2003-2013). Earned Ph.D from Japan (1993-1997). My Researches have been focused on the developing and application of analytical techniques in the field of toxicology, drug toxicokinetics , genotoxicity of nanoparticles and neurodegenerative diseases therapeutic approaches from natural origin . Lately published a number of articles in toxicological assessments of nutraceuticals. Involvement in national & international projects in cooperation with industry, to solve current problems or to innovatively develop market driven products form natural sources such as ; Combating Stunting in Qaliubia Egypt (CO PI, financed by Misr El Kheir Foundation). Rice bran Nutraceuticals and Rice Bran innovative formulation (Partner, Financed by the EU). Pharmaceutical Pectin from Orange Peels (Consultant, financed by Science and Technology Development Fund).
Abstract:
It is estimated that more than 500000 Tons of rice bran is produced in Egypt every year. Though its nutritional values and potential health benefits, it is used , due to its instability , as animal feed rather high value functional food and/ or high value added nutraceuticals. A number of papers were published showing, the stabilized rice bran extract, potential health benefits in some diseases like Alzheimer’s disease (Hagel et al., 2013 2015 a,b, c). The product is registered (Oryza), another one under registration at the Egyptian Ministry of Health (Riciplex) . A functional food against Alzheimer is currently developed in Germany, based on the Stabilized Egyptian rice bran supplied (Porridge Plus 6). In the present study the effects of RBE were examined in comparison to a well-known PPARγ agonist pioglitazone. RBE administration significantly improved the spatial working and reference memory in addition to non-spatial recognition memory in the LPS mouse model as shown by object recognition test, y-maze and water maze test. Pioglitazone improved memory, in the Y-maze and object recognition test with no effect in the water maze test. Interestingly, the effect of RBE on memory was abolished in the group injected with PPARγ-antagonist before RBE treatment, indicating the important role of PPARγ in the mechanism of action of RBE. Furthermore, the RBE -PPARγ DNA binding activity was measured in the brain extract samples of the mouse treated groups using transcription factor assay kit. Results showed a significant increase in PPARγ binding to PPRE with RBE treatment and this effect was reversed upon PPARγ antagonist injection before RBE treatment. These findings demonstrate that the involvement of RBE in the beneficial effects on cognitive performance is correlated with its action on PPARγ modulation, providing novel insight into its neuroprotective role in AD.
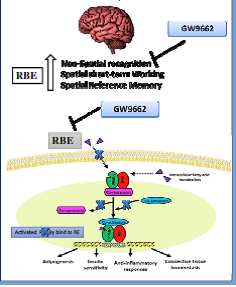
Koorosh Shahpasand
Royan Institute for Stem Cell Biology and Technology, Iran
Title: A Major Early Driver Of Tauopathy And Neurodegeneration That Is Blocked By Antibody

Biography:
Abstract:
Mona H Tawfik
Beni suef University, Egypt
Title: Cognitive Functions in Patients with Parkinson’s Disease: I. The Effect of Cerebral Microstructural Changes

Biography:
Mona Hussein Tawfik, has Master and MD degree in neurology from neurology department, Cairo University. She works as a neurology lecturer in Beni suef University. She has her expertise in evaluation and assessment of cognitive impairment. She has built her knowledge after years of experience in research in cognition. She has many publications about cognitive impairment in Parkinson's disease, Alzheimer's disease and normal aging.
Abstract:
Cognitive impairment in Parkinson’s disease (PD) was extensively studied in the medical literature. Correlating such cognitive impairment with the macro and microstructural changes in cerebral grey and white matter, has gained more attention in the last years. Aim: To explore the cognitive profile of patients with PD and to correlate the brain atrophic changes and the microstructural changes in cerebral grey and white matter with the cognitive pattern in Parkinson's disease. Subjects and methods: The study was conducted on 40 patients with PD and 20 controls. Selected PD patients were submitted to evaluation of cognitive function using PD-Cognitive Rating Scale (PD-CRS), and assessment of microstructural changes in substantia nigra (SN), caudate, putamen, globus pallidus (GP), thalamus, hippocampus and prefrontal white matter using diffusion tensor imaging (DTI). Results: The cognitive impairment in PD patients starts with executive dysfunction followed by impairment in attention, episodic memory, and visuospatial skills. Naming is the last cognitive domain to be affected in PD patients. The cognitive impairment in PD patients can be attributed to the microstructural changes (decreased Fractional anisotropy) in SN, caudate, putamen, GP, thalamus, hippocampus and prefrontal white matter. Conclusion: Cognitive impairment in PD is present even in the earlier stages of the disease and it can be correlated with the microstructural changes in SN, caudate, putamen, GP, thalamus, hippocampus and prefrontal white matter
- Track 2:Neural Stem Cell | Track 3:Neuroethics | Track 12:Molecular Neuropharmacology | Track 13:Future Aspects of Neuropharmacology | Track 14:Case Study Reports
Session Introduction
Hua P Su
MSD Research Labs, USA
Title: Characterization of non-active site, TrkA selective kinase inhibitors and implications on obtaining kinase selectivity

Biography:
Hua P Su has expertise in structure based drug discovery with a focus on using x-ray crystallography to understand mechanism of action and inhibition. Having worked on numerous drug discovery projects including multiple neuroscience targets with small molecule and biologic modalities, he is interested in identifying new mechanisms of interaction that provides specificity to the targets and how to design screens that address selectivity.
Abstract:
Current therapies for chronic pain can have insufficient efficacy and lead to side effects, necessitating research on novel targets against pain. Although originally identified as an oncogene, TrkA is linked to pain and elevated levels of NGF, the ligand for TrkA, are associated with chronic pain. Antibodies that block TrkA interaction with its ligand, NGF, are in clinical trials for pain relief. Here, we describe the identification of TrkA-specific inhibitors and the structural basis for their selectivity over other Trk family kinases. The x-ray structures reveal a novel binding site outside the kinase active site that utilizes residues from the kinase domain and the juxtamembrane region. Three modes of binding with the juxtamembrane region are characterized through a series of ligand-bound complexes. The structures indicate a critical pharmacophore on the compounds that leads to the distinct binding modes. The mode of interaction can allow TrkA selectivity over TrkB and TrkC or promiscuous, pan-Trk inhibition. This highlights the difficulty in characterizing the structure-activity relationship of a chemical series in the absence of structural information due to substantial differences in the interacting residues. These structures illustrate the flexibility of binding to sequences outside of, but adjacent to, the kinase domain of TrkA. This knowledge allows development of compounds with specificity for TrkA or the family of Trk proteins and has implications on obtaining selectivity for kinase targets in drug discovery.

Biography:
Jan Ulfberg, MD, PhD, Sleep Disorders Center, Läkargruppen, Örebro, Sweden, has been dedicated to sleep research during recent thirty years, with a special interest in restless legs syndrome ( RLS ), even named Willis Ekbom Disease ( WED ). The main focus of this research has been on the epidemiology and the pathophysiology of this disease.
Abstract:
Mathew Nguyen
Meridian Behavioral Healthcare, USA
Title: Combination Brexpiprazole and Aripiprazole Long-Acting Injectable Therapy for Treatment-Resistant Schizophrenia

Biography:
Mathew Nguyen, MD, MBA is board certified in Adult Psychiatry and Child/Adolescent Psychiatry. He recently retired from faculty at the University of Florida, where during his 15 years, he oversaw multiple divisions, including Child/Adolescent Psychiatry, Consultation/Liaison, Medical Psychology, and Eating Disorders. Dr. Nguyen currently runs an adult psychiatry inpatient unit at Meridian Behavioral Healthcare, Inc. in Gainesville, Florida. He continues to be involved in clinical research, lecturing, and publishing. He also recently graduated from the University of Florida with a Masters in Business Administration and plans to incorporate the MBA into improving patient care models.
Abstract:
Schizophrenia has a prevalence rate of 1% and is a complicated illness that often leads to periods of relapses. Up to a third of patients with schizophrenia are considered to be treatment-resistant. Despite the new and various antipsychotic medications that have recently come to market, the number of treatment-resistant cases continue to abound. This has led to a sub-population of patients with schizophrenia being treated with more than one antipsychotic medication concurrently. Though it has become more common in clinical practice, there is sparse literature to objectively support the combination use of antipsychotic medications. There is also little literature addressing the use of a long-acting injectable (LAI) used in combination with another atypical antipsychotic. This case report serves to highlight the concurrent use of aripiprazole LAI used in combination with oral brexpiprazole in two patients with treatment-resistant schizophrenia. The receptor binding affinity of these two antipsychotics appear complementary and perhaps even protective for extra pyramidal symptoms (EPS). We hypothesize that the use of a LAI serves as a “foundational barrier” to mitigate the potential for full psychotic relapses should patients become noncompliant with their oral medications, and that the LAI also may help with oral medication compliance in this subpopulation of treatment-resistant schizophrenia patients by increasing baseline functionality.

Biography:
Maha Ali Nada, I am a fourty one years old assistant professor of neurology in Ain Shams University which is one of the greatest univesitiesies in Cairo. Graduated in 1999. I' ve been practicing neurology since 2001 as resident , assistant lecturer, lecturer, and assist prof since 2014. My MD thesis was namd: Clinicoradiological localisation of language disorders in acute ischemic CVS. I joined multiple sclerosis section in our department for 7years during which, I was responsible for day therapy care for all MS patients in our department. I used to attend all neurological conferences and to participate as speaker in some. 2 years ago, I became responsible for the pediatric neurology clinic in my department, which is a specialized afternoon clinic. Being the most senior in the clinic, it was my duty to teach younger staff and to encourage them to attend this new clinic which soon became the largest of the specialized clinics in our department regarding the number of patients attending(40 patients/clinic). Trying to register this large number of patients, we find many candidates for case reports and many ideas for new research. I 've also published a case report in the BMJ (British Medical Journal) on 12/2015 with a group of medical students and I was their mentor. Many puplications in the Egyptian Journal of Neurology, psychiatry and neurosurgery.One paper in the Journal of American Science in 2012
Abstract:
Among causes of secondary enuresis, epilepsy was none of those. It was observed in 15 children with secondary enuresis whom were urologically free, that their sleep EEG showed epileptic discharge without any other manifestations of epilepsy. After receiving antiepileptics, soon they became dry. There were common manifestations between those patients and they share some EEG similarities which we will try to explain aiming to shed the light on this possible new syndrome. This can guide future research for better management of such condition.
Saule T.Turuspekova
KazNMU, Kazakhstan
Title: Tanakan (EGb 761®): new therapeutic possibilities in neurorehabilitation

Biography:
Saule T.Turuspekova MD, PhD, neurologist highest category, Professor of the Department of neurology and Neurosurgery of KazNMU. 1995- PhD Thesis -"Vegetative-vascular disorders in cerebral manifestations of diabetes mellitus." 2010 - Doctoral thesis - "The influence of small doses of ionizing radiation on the nervous system". Over 130 scientific papers which were presented at international conferences in many countries. State scholarship for talented young scientists of the Ministry of Science of the Republic of Kazakhstan. Coordinator of the Russian Youth Academy of Sciences (Samara). 2015-the personal physician of the Kazakhstan astronaut Aydin Aimbetov. Medal "Success of the Year". Badge and certificate of "Pride of the University" for outstanding contribution to the development of healthcare and medical science of the Republic of Kazakhstan and strengthening the image of the university. Patent holder The patent for invention number 31607The method of treatment patients with ischemic stroke in the early recovery period. The patent for invention number 31742The method of treatment patients with spinal cord injury in early rehabilitation period. Member of the ESO, WSO, EAN.
Abstract:
There is an opinion that an insufficient level of external magnetic effect in terms of the degree of harm to the body can fully compete with a deficiency of minerals and vitamins, a prolonged stay in a weakened magnetic field of the Earth has a depressing effect on the central nervous system.Recently, more and more attention of researchers has been attracted to the neurostimulating effect of pulsed magnetic fields, in particular transcranial magnetic stimulation.
Objective: To evaluate effectiveness of ion-reflex induction magnetophonophoresis session using Extract of Ginkgo biloba (Tanakan (EGb 761®)) in rehabilitation of patients with ischemic stroke in the early recovery period.
Materials and methods: 72 patients were supervised with ishemic stroke. The bioelectric activity of the cerebral cortex (EEG) was studied. There were use Mini Mental State Examination (MMSE), The Montreal Cognitive Assessment Scale (MoCA), and Barthel ADL Index. Quality of life was assessed by questionnaire Rivermead. Under observation were 3 groups: 1st- 49 patients who received an extra ion-reflex induction magnetophonophoresis sessions using Extract of Ginkgo biloba (Tanakan (EGb 761®)) by applying head’s frontooccipital longitudinal galvanization techniques were conducted; 2rd- 23 patients treated with protocol formed without sessions, 3rd -25 healthy volunteers aged 21 to 70 years.
Results: sessions of ion-reflex induction magnetophonophoresis using Extract of Ginkgo biloba (Tanakan (EGb 761®)) longitudinal methods fronto-occipital head galvanizing can achieve more significant results. There was a significant positive dynamics of cognitive functions according to the MoCA test in the intervention group (from 20,0 ± 2,3 to 26,8 ± 2,3 points) compared with controls (20,2 ± 2,1 - 23,2 ± 2,1). The MMSE was not informative. Barthel index rose by 10 points, Rivermead -15, respectively, in the 2nd - without dynamic. The EEG noted a decrease in interhemispheric asymmetry of the α-rhythm in amplitude by 30-55% in 95% of patients, reducing the severity of slow-wave shifts by 30-40%. Expression and modulation of α-rhythm improved in 90% of cases. In dynamics, the slow wave activity decreased in 85% of patients.
Conclusions: The research’s indicators’ dynamics shows positive impact of ion-reflex induction magnetophonophoresis sessions using Extract of Ginkgo biloba (Tanakan (EGb 761®)) by applying head’s frontooccipital longitudinal galvanization techniques in rehabilitation of patients with ischemic stroke in the early recovery period.
Giuseppe Scalabrino
University of Milan, Italy
Title: The molecular basis of the neurotrophic action of vitamin B12 (cobalamin)

Biography:
Giuseppe Scalabrino studied at the School of Medicine of the University of Milan and received his M.D. degree magna cum laude in 1968. He has held a number of academic positions in the Faculty of Medicine of the University of Milan. He was Associate Professor of General Pathology between 1971 and 1985; full Professor of General Pathology from 1986 till 2014. He has been invited speaker in various conferences, mainly dealing with the role of polyamines in oncology and subsequently with the cobalamin (vitamin B12) neurotrophism. Among his numerous honors, he received the International Award "Roentgen" from Italian Accademia dei Lincei in Rome for oncological research in 1983. He is author of more than 100 scientific papers and reviewer of numerous International Journals. Dr. Scalabrino's studies of cobalamin neurotrophism have been mentioned and reviewed in 12 american textbooks of neurology, biochemistry, hematology, and vitaminology.
Abstract:
Our experimental and clinical studies have highlighted the non-coenzyme functions of cobalamin (Cbl, vitamin B12). Cytokine and growth factor (GF) imbalance in the central nervous system (CNS) of Cbl-deficient (Cbl-D) rats is a key point in the pathogenesis of Cbl-D neuropathy. The increased molecules are tumor necrosis factor(TNF)-a, nerve GF, and the soluble (s) CD40:sCD40Ligand dyad; the decreased molecules are epidermal GF (EGF) and interleukin-6. The in vivo administration of the lacking myelinotrophic molecules or agents antagonizing the excess myelintoxic agent is as effective as Cbl in repairing or preventing Cbl-deficiency-induced CNS myelin lesions. Cbl deficiency morphologically affects also glial cells, which normally synthesize and release various cytokines and GFs. Therefore, Cbl deficiency triggers the rearrangements of glia gene expression, eventually leading to a changed pattern of cytokine and GF production. Such an opposite imbalance in TNF-a and EGF similar to that observed in CNS of Cbl-D rats has been found in the sera of adult patients with pernicious anemia (but not in patients with iron-deficient anemia), and it was rectified by Cbl therapy. This imbalance has been found also in the cerebrospinal fluid (CSF) of adult patients with Cbl-D neuropathy. Given that TNF-a and EGF regulate the expression of normal prions (PrPcs) and PrPcs play a crucial role in myelin maintenance, we investigated whether CNS PrPc levels are indirectly regulated by Cbl. PrPc levels had increased by the time Cbl-D-induced myelin lesions appeared. This increase was mediated by excess TNF-a and prevented by EGF. Cbl deficiency greatly reduced CNS PrPc-mRNA levels, which were subsequently increased by Cbl and EGF. Similar increases in PrPc levels also occur in the serum and CSF of adult Cbl-D patients, and the serum increase has been corrected by Cbl therapy. Therefore, Cbl may regulate the PrPc levels in the serum and CSF in humans.
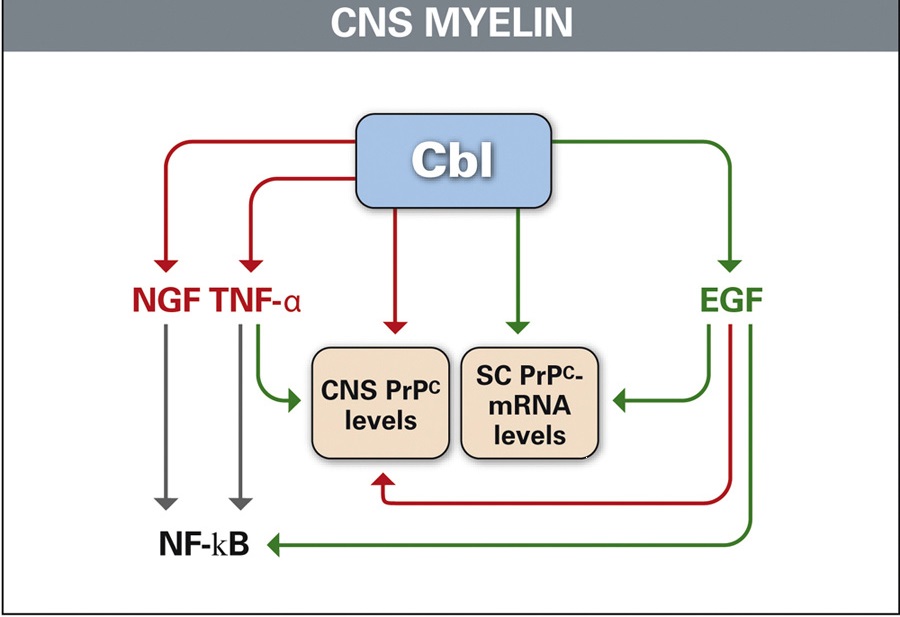
Figure 1: Cbl as a fulcrum between physiologically myelinotrophic (green) and potential myelinodamaging agents (red) in rat CNS. This is highlighted by the Cbl-mediated stimulation of EGF, the Cbl- and EGF-mediated stimulation of PrPc synthesis (green arrows), and the reduction of TNF-a and NGF levels (red arrows), eventually leading to a low NF-kB level
Natalia Malikowska
Jagiellonian University Medical College, Poland
Title: Studying the effectiveness of venlafaxine in mice model of post-traumatic stress disorder

Biography:
Natalia Malikowska is a PhD student at the Jagiellonian University Medical College. Besides fulfilling herself in a Pharmacy, she also realizes her scientific passion working at the Department of Pharmacodynamics, Faculty of Pharmacy CM UJ as a Behavioral Pharmacologist. Previously she was working on Epilepsy and Pain Issues, but nowadays her area of expertise has been expanded to memory, depression and PTSD studies. She is a young, but very creative researcher with really strong need to broaden her knowledge. Pretty long period of belonging to students’ scientific group enabled her to get acquainted to the laboratory and working with animals, also acquired academic achievements.
Abstract:
Statement of the Problem: Posttraumatic stress disorder (PTSD) is a psychiatric disease, associated with excessive stress and anxiety due to the cues which provoke re-experiencing of traumatic events. Because in PTSD we observe symptoms associated with depression and anxiety, the current pharmacotherapy includes antidepressants (mainly serotonin reuptake inhibitors, SSRIs) and anxiolytic drugs (benzodiazepines). However, these drugs are ineffective in some individuals. Furthermore, adverse effects of the above-mentioned drugs, in particular benzodiazepines, strongly impair patients’ social life. Our study was performed to determine if drugs acting via other neurotransmitter systems might present a higher activity in the mouse model of PTSD. For this purpose we studied the efficiency of venlafaxine, an antidepressant drug that interacts with serotoninergic, noradrenergic and dopaminergic pathways.
Methodology & Theoretical Orientation: The mouse model of PTSD was induced using single prolonged stress protocol (mSPS). The effectiveness of venlafaxine was assessed using the forced swim test (FST) 24 h, 3 days, 8 days, 15 day and 25 days after mSPS. In order to compare the activity of venlafaxine in PTSD model to its antidepressant effect in non-PTSD conditions, we have also performed FST in naïve mice.
Findings: Venlafaxine, when compared to SPS-subjected control group, presented antidepressant activity in the repeated FST, except for the day 8th (Fig. 1). The highest activity was observed on day 25, which correlates with findings that SPS model requires up to 3 weeks to become fully developed. However, when venlafaxine was tested in naïve mice, strong, antidepressant effect was demonstrated.
Conclusion & Significance: Venlafaxine is an effective drug in the mouse model of PTSD, although presented effect increases gradually. PTSD might induce neurobiological changes which cannot be fully reversed by venlafaxine administration, which is confirmed by higher activity of venlafaxine in non mSPS-subjected mice.
Rebeillard Florian
Université Paris Descartes, France
Title: Developmental and adult expression of the GPR88: Establishment of its interaction with nuclear partner proteins in the cerebral cortex

Biography:
Rebeillard F is a Doctor in Pharmacy and a first year PhD student. With his Medical and Scientific training his area of expertise includes pharmacology and health while integrating both fundamental science/research and patients care. This distinctive project about the unusual working principle of a nuclear GPCR is motivated by the need of supporting fundamental/academic research, and hopefully providing new openings for psychiatrics treatments to improve patients’ lives.
Abstract:
GPR88 is a neuronal orphan G-protein-coupled receptor preferentially concentrated in synaptic sites of the GABAergic MSNs, highlighting a neurotransmission role for GPR88 in MSNs which play a central role in a wide array of psychomotor functions subserved by the basal ganglia. However, no extensive description of its developmental expression has been provided so far. We reported that GPR88 protein is initially detected at embryonic day 16 (E16) in the rat striatal primordium. From E16-E20 to adulthood, the highest expression levels of both protein and mRNA are observed in striatum, olfactory tubercle, nucleus accumbens, amygdala, and neocortex. We also observed an intracellular redistribution of GPR88 during cortical lamination. In the cortical plate, GPR88 presents a classical GPCR plasma membrane/cytoplasmic localization that shift, on the day of rat birth, to nuclei of neurons progressively settling in layers V to II. This intranuclear localization remains throughout adulthood and was also detected in mouse, monkey and human cortex. Transfections of GPR88 fluorescent chimeras into the rat cortical neurons demonstrated that nuclear localization depends on the I3 and C-terminus domains. GPR88 protein has no known NLS motifs, suggesting that GPR88 is driven into the cell nucleus by partner proteins. A yeast two-hybrid screen on a mouse brain cDNA library enabled to identify nuclear proteins including ATRX, TOP2B and BAZ2B as potential partners of GPR88. The results of proximity ligation assay experiments on neuronal cultures of cortex from WT and KO-GPR88 mice have validated the interaction of GPR88 with these nuclear proteins which are involved in the chromatin remodeling. The current description of the GPR88 subcellular expression may provide precious functional insights into this novel receptor. Furthermore, the GRP88 nuclear localization suggests nonclassical GPCR modes of action of the protein that could be relevant for cortical development and psychiatric disorders.
Gafarov Valery
Collaborative laboratory of cardiovascular diseases epidemiology, Russia
Title: Association of polymorphism rs2412646 clock gene with some socio-psychological features and sleep disorders in male population 25-44 years in Russia / Siberia

Biography:
Professor Gafarov Valery, in 1974 - MD (Novosibirsk medical university). 1980 - Phd, theme " Epidemiological studying Acute Myocardial Infarction in conditions of large industrial centre of Western Siberia". 1991 - MPH; 2003 - professor on a specialty "cardiology"; 2003 - present time – head of collaborative laboratory of epidemiology cardiovascular diseases and Laboratory of psychological, sociological aspects of therapeutic diseases of Research Institute of Internal and Preventive Medicine. The author of 758 scientific publications (articles and abstracts), from them 6 monographs
Abstract:
Objective: to study the prevalence and association of rs2412646 gene CLOCK with some components of the socio-psychological characteristics and sleep disorders in the male population 25-44 years in Russia / Siberia (Novosibirsk).
Materials and methods. In 2014-2016 GG It surveyed a random representative sample of the male population 25-44 years, one of the districts of Novosibirsk. Randomly selected 200 men had a mean age of 35.5 years, who underwent psychosocial testing. Testing conducted by questionnaire "4-item Jenkins Sleep Questionnaire». Test anxiety and depression conducted modified questionnaires of the Welsh Depression subscale of the MMPI and Bendig Anxiety subscale of the MMPI, the study of the life of exhaustion conducted questionnaires The Maastricht Questionnaire (MQ). Questionnaire "Awareness and attitude towards their health" was also proposed. The men included in the study, studied the frequency distribution of genotypes of rs2412646 CLOCK gene. Differences in the distribution of genotype frequencies CLOCK gene were evaluated by Chi square (X2) test between groups. The values of p ≤ 0,05 were considered statistically significant.
Results. It was found that the most common genotype in the population was the C / C gene CLOCK -50,3%, C / T met at 42.5% and genotype T / T all at 7.2%. Most of the men were of the opinion, that would be addressed to the doctor only when severe pain or discomfort in the heart, but would not return if the pain or discomfort would be poorly expressed, however, 10.7% of men, the carriers of the genotype C / T, I would not go to a doctor, even when a severe pain or unpleasant sensations in the heart. It is also more likely to have continued to work carriers of genotype C / T - 47,4%. Among the carriers C / T genotype often sounded that their sleep is "satisfactory" or "poor." Media C / T genotype, compared with carriers of other genotypes, most agreed with the statement that oppresses them in a bad mood, and they are much less careful and attentive to detail.
Conclusion: Our results indicate a correlation between the presence of social and psychological factors, and sleep disorders, and polymorphic markers rs2412646 CLOCK gene.
Kadhim Alabady
Public Health and Safety Department - Dubai Health Authority (DHA), UAE
Title: Assessing Autism Spectrum Disorders (ASD) Challenges among Children in Dubai – Mixed research approach – (Triangulation of data), 2016

Biography:
Hold a Doctorate degree in Public Health and Epidemiology, Master degree in Clinical Epidemiology (MSc), Master degree in Public Health (MPH), all from The Netherlands Universities.
· Worked in Public Health since 1999 at different levels such as:
- Academic (Erasmus university – Rotterdam / The Netherlands, Queen Marry University – London / UK), University of East Anglia UEA / Norwich.
- International (United Nations).
- National Health Authority (Qatar).
- National Health Service (NHS), UK since Feb 2007.
- others
· Registered as Epidemiologist Grade A with The Netherlands Epidemiological Society.
· Has numerous publications in the UK in mental illnesses, cancer, cardiovascular diseases, diabetes, Dementia, Autism, COPD, population health, road casualties and others.
· Has broad experience with a wide variety of statistical software programs i.e. SPSS, STATA, excel, etc.
· Broad experience of R&D.
· Designing, conducting, analysing, and presenting quantitative and qualitative researches.
Abstract:
Background: Autism poses a particularly large public health challenge and an inspiring lifelong challenge for many families; it is a lifelong challenge of a different kind. Purpose:
Purpose: To understand what are the key challenges and how to improve the lives of children who are affected with autism in Dubai.
Method: In order to carry out this assessment we have used two approaches:
- Qualitative methodology (focus groups with mental health experts working at: Al Jalila hospital (AJH), Dubai Autism Centre (DAC), Dubai Rehabilitation Centre for Disabilities, Latifa hospital, Private Sector Healthcare (PSH).)
- Quantitative methodology. Prevalence or incidence estimates based on international research.
Key findings:
- Autism is the most common of the Pervasive Developmental Disorders. Dubai Autism Center estimates it affects 1 in 146 births (0.68%). If we apply these estimates to the total number of births in Dubai for 2014, it is predicted there would be approximately 199 children (of which 58 were Nationals and 141 were Non–Nationals) suffering from autism at some stage.
- Autism spectrum disorder (ASD) is a public health concern in Dubai. Families do not consult GPs for early diagnosis for a variety of reasons including cultural reasons.
Recommendations:
- Training of GP’s to aid early diagnosis of Autism and increase awareness.
- There is an urgent need for an adult autism center for when the children leave the safe environment of the school at 18 years.
- There is a need for further studies to cover the needs of people with an Autism Spectrum Disorder (ASD).
Mansoureh Togha
Tehran University of Medical Sciences, Iran
Title: Headache in relapse and remission phases of multiple sclerosis: A case-control study

Biography:
Mansoureh Togha received MD from shiraz university of medical sciences(1998) and graduated in course of specialty in “Neurology” in 1993 from the Tehran University of Medical Sciences(TUMS). Since then,she has been working as professor of neurology at TUMS. She is most interested in headache and facial pain researches. She has many experience of research, evaluation, and teaching in this field both in university hospital and private clinic. Also she has been the supervisor and advisor of more than 50MD, PhD and MSc theses and of a large volume of research works in collaboration with various research centers. Her main topic of research includes evaluating mechanisms involved in migraine development and progression, examining new treatment strategies and assessing the rate of comorbid disorders aimed at alleviating different types of headaches specially migraine. She has co-authored over50 international peer-reviewed publications and presented about100 papers and lectures at national or international scientific conferences.
Abstract:
Statement of the Problem: Characterization of headaches and delineating possible relationships with Multiple Slerorosis(MS)-related determinants can ultimately circumvent headaches. Thus, in this study, we attempted to assess the prevalence of headaches during relapses and remissions of relapsing-remitting MS(RRMS)patients and denote the possible interrelations between headaches and types of MS exacerbations.Methodology & Theoretical Orientation: In a prospective case-control study, 65 RRMS patients and 65 healthy controls were recruited and asked about characteristics and co-symptoms of headaches they experienced in the preceding week and usage of disease modifying drugs and types of MS attacks were also inquired. The same questions were asked from the same patients 3 months later in a follow-up visit. Findings:A total of 57patients and 57controls were included in the final analyses. In total,26(45.6%) patients in relapse, 18(27.7%) controls, and 22(38.6%) patients in remission reported headaches and only significant difference existed between relapse patients and controls(P = 0.036). The headache prevalence was higher in patients in relapse phase having MS<3years compared to relapse patients with>3years of MS (68vs. 28.1%;P = 0.004). Other variables of interest did not differ among the three groups. Conclusion &Significance:The suggested explanation for migraine-MS interrelationship is that migraine, especially migraine with aura, switches on particular matrix metalloproteinases that in turn destruct the blood-brain barrier and render myelin autoantigens vulnerable to autoreactive T-cells present in the bloodstream and this process can ultimately culminate in MS. Furthermore, migraine episodes and MS attacks apparently share common cytokine profiles. According to our study at the earlier stages of MS, headaches were more common during attacks which may be due to active immune process in that stage. Common genetic and environmental determinants present in MS, and headaches are also on the agenda of headache-MS association. In summary, The RRMS patients in relapse phase suffer from headaches more than healthy people do.
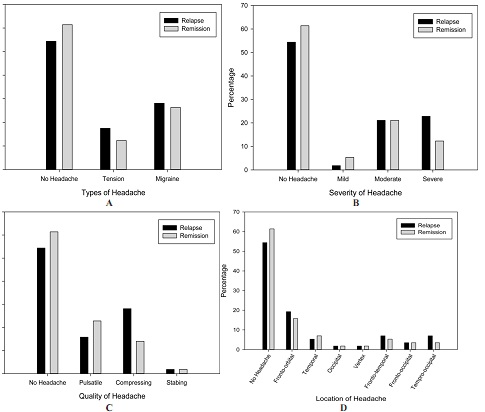
Figure 1. Features of headache attacks during relapse and remission phases among patients with relapsing-remitting multiple sclerosis, (A) Types of headache, (B) severity of headache, (C) quality of headache, (D) location of headache
- Special Session
Session Introduction
Yacov Rofé
Bar-Ilan University, Israel
Title: The Intuitive Rational-Choice Theory of Madness: Schizophrenia, Criminal Insanity & Neuroses The Fallen Empires of Psychoanalysis, Medical Models and Drug Companies

Biography:
Yacov Rofé is a professor of psychology at Bar-Ilan University, Ramat-Gan, Israel. He completed his first and second degrees in psychology at Bar-Ilan University and received his Ph.D. from Hull University, England, in 1973. He held the position of chair of the interdisciplinary department of social sciences at Bar-Ilan University for fifteen years. Rofé was a visiting professor at both Rutgers Medical School in New Jersey and Washington University in St. Louis, Missouri.
He has published many articles in leading academic journals of psychology, including a theory entitled “Stress and Affiliation: a Utility Theory”, published by Psychological Review in 1984. An additional influential article, published in Review of General Psychology, 2008, is a review that refutes the existence of repression and the Freudian Unconscious.
In recent years, Rofé’s scientific work has focused on the development of a new theory of psychopathology, which challenges the validity of traditional theories of psychological disorders. Rofé published a book entitled The Rationality of Psychological Disorders, by Kluwer, in 2000. He has since published four subsequent articles supporting his Rational-Choice Theory of Neurosis (RCTN). These include articles which : (1) demonstrates the ability of RCTN to integrate all therapeutic methods pertaining to neurosis in one theoretical framework (Rofé, 2010), (2) integrates all data relevant to the development and treatment of conversion disorder (Rofé & Rofé, 2013), (3) resolves the theoretical confusion regarding the explanation of panic disorder, agoraphobia and other forms of bizarre phobia (e.g., chocolate phobia) (Rofé, 2015), and (4) that suggests a new diagnostic criteria based on RCTN that challenges the validity of the DSM (Rofé, 2016).
Rofé completed a new book, entitled The Intuitive Rational-Choice Theory of Madness: Schizophrenia, Criminal Insanity and Neurosis: The Fallen Empires of Psychoanalysis, Medical Models and Drug Companies. Distinguished researchers, including Professor Robert Aumann, Nobel Prize Winner in economics, acknowledged the merits of this book. In his letter to the editors, Aumann noted, "Rofé's theory, revolutionary as it is, fits well into the framework of economics, game theory and evaluation."
Abstract:
The book, The Intuitive Rational-Choice Theory: Schizophrenia, Criminal Insanity & Neuroses, presents a new theory, which explains the development and treatment of schizophrenia and criminal insanity as rational coping mechanisms. It demonstrates the widespread conviction that schizophrenia is a brain disease, which is primarily due to the weaknesses of psychological theories explaining the strong relationships between schizophrenia and neurological impairments. Consequently, medical models took for granted that all cases of schizophrenia result from brain disease, even when there was no evidence for neurological impairments, as in the case the Unabomber and John Nash. This new theory reverses the method of investigation: It first explains case studies with no evidence of brain impairments and then generalizes it to research where clear-cut evidence of such impairments were found. Using this methodology, it is demonstrated that the new theory can explain all cases of schizophrenia, as well as numerous cases of criminal insanity and neurotic disorders, along with the variability of the stark differences between the various cases, as rational coping mechanisms.
According to this new theory, when individuals are confronted with extreme levels of stress, regardless of whether the source of the stress is neurological or environmental, their behavioral options become limited: They can commit suicide, develop a drug abuse, use aggression to eliminate the stressor, or intuitively choose certain mad behaviors that suite their coping demands. Madness is defined by five major diagnostic criteria: The behavior must intensively preoccupy the individual's attention and disrupt his daily functioning, onset must be in the absence of observable events that are uniquely associated with this behavioral change, it must be rare, the patient should be unaware of the underlying causes for the behavioral change and it must be socially stigmatized as abnormal or bizarre. Mad behaviors are categorized to neuroses or psychoses, based on presence or absence of delusions, hallucinations and disorganized speech (see Rofé, 2016).
Madness is seen primarily as a repressive coping mechanism, which individuals intuitively/unconsciously choose when confronted with unbearable levels of stress. The choice of a specific behavior is determined by the same three principles which guide the consumer's decision-making process when purchasing a certain product (e.g., see Wänke & Friese, 2005). The major principal is the need for the specific product/symptom, which in madness is controllability. The specific behavior must increase the patient's ability to exercise control over the stressor andor provide certain desired privileges. The second guiding principle is availability, which indicates that the choice of a specific symptom is affected by various channels of information, such as the media, personal experiences, genetic predispositions, family and peers that increase the saliency of certain suitable behaviors (see Rofé, 2000). The third principle is cost-benefit analysis, which states that a mad behavior may only be chosen if the individual intuitively feels that it will reduce the level of his or her emotional distress.
Although the decision to implement the intuitive/unconscious choice is conscious, patients become unaware of the Knowledge of Self-Involvement (KSI), or the True Reason (TR) for acting bizarrely through a variety of cognitive processes that disrupt the encoding of this knowledge and memory-inhibiting mechanisms that cause its forgetfulness. Subsequently, utilizing their socially internalized beliefs regarding the causes of psychological disorders, patients develop a self-deceptive belief which attributes the cause of their symptoms to factors beyond their conscious control, and thus stabilizes the unawareness of KSI/TR.
The new theory proved its ability to integrate all therapeutic methods pertaining to neurosis into one theoretical framework (Rofé, 2010), explaining all data relevant to the development and treatment of conversion disorder, including neurological findings, which seemingly support the medical explanation of this disorder (Rofé & Rofé, 2013), and resolves the theoretical confusion regarding the explanation of phobia by distinguishing between a bizarre phobia (e.g., agoraphobia, and chocolate phobia) and non-bizarre phobia, such as dog phobia (Rofé, 2015). Robert Aumann, the Nobel Prize-winning economist, noted in a letter of recommendation to publishers of the present book (2017), Rofé's theory is as "revolutionary as it sounds, fits well into the frameworks of economics, game theory, and evolution".
- Track 4:Clinical Neuropharmacology | Track 5:Psychopharmacology | Track 7:Behavioral and Addiction Neuropharmacology | Track 8:Neurotechnology
Session Introduction
Oscar Bernal-Pacheco
Instituto Roosevelt, Colombia
Title: Deep brain stimulation for uncontrollable aggressive behavior, The benefit beyond our expectations

Biography:
Oscar Bernal-Pacheco obtain his medical degree of the Universidad Nacional de Colombia, Neurologist of the Universidad Militar (Colombia) and fellow of the University of Florida at Gainesville (USA). Currently he is professor of the Universidad Militar, Hospital Militar from Bogotá (Colombia), co@director of the movement disorders clinic in the Hospital Fundación Santafe de Bogotá and Instituto Ortopedico Roosevelt. He have been working in Deep Brain Stimulation for patients with movement disorders such Parkinson’s Disease but also for neuropsychiatric conditions. The wide clinical response to DBS has become the base to look for more than motor benefit in movement disorders and is more than previously described non@motor changes.
Abstract:
Deep brain stimulation is a procedure available for movement disorders, and for some psychiatric conditions non responding to pharmacological options such aggressive and uncontrollable behavior.
A woman with perinatal hypoxia, delay of milestones and severe mental retardation, developed hyperfagia, severe impulsivity with uncontrollable aggressive behavior, she was always under surveillance, required phisycal restriction and she was isolated in her house, being dependant in all activities of daily living. The second patient is a man, 24 years old, with severe mental retardation, impulsivity and uncontrollable aggressive behavior, hitting even his parents and anybody nearby. He also has epilepsy with frequent seizures. The last patient is an 18 year@old man, with normal development. At the age of 14, he presented generalized epilepsy. Since then, his behavior tends to be aggressive and impulsive, manifesting in worsening epilepsy and aggressive behavior. All three patients received multiple medications including antipsychotics and antiepileptics. Due to the persistence of symptoms, every case was discussed in a multidisciplinary team, supported by the criteria for DBS for agressive behavior, and the ethical committe agreed on a deep brain stimulation in the posterior medial hypothalamus.
Criteria for DBS for agressive and uncontrollable behavior includes: to be diagnosed by two psychiatrists, non@response to treatment despite the highest dosage of at least five antipsychotic medications in an enough period of time to evaluate the response and the severe functional interference with the activities of daily living and malanadaptative behavior. All patients showed improvement after the procedure. The woman was released of physical restriction and she can now go with her family out of her house without being a risk for herself or for others.
The benefits of the second case included control not only of the behavior but also of seizures, diminishing medications for aggresive behavior and also for epilepsy. In this case, voltage over 3,4 V showed hypoactivity, with hyporexia, becoming extremely undernourished and requiring the reduction of the voltage to 3,2 V.The third case showed benefit and he could go back to school again, being able to control his aggresive behavior as well as the epilepsy. The benefits amount to around 70% in all cases, with parameters of stimulation between 3 and 3,4, pulse width of 60 and frequency of 130.
Conclusion: DBS in the posterior medial hipothalamus can be an usseful option in the control of uncontrollable aggressive behavior. We also found benefit with better control of seizures in two patients with epilepsy.
Arieh S Solomon
Tel Aviv University , Israel
Title: Prolonged inhibition of semaphorin3a pathway via biodegradable implant towards a better therapy for visual sensory impairments

Biography:
Arieh S Solomon initiated research in studying the degeneration and regeneration process of the optic nerve , following assaults. He concepted a new type of intra ocular implant to treat glaucoma (the blinding disease creating high IOP and killing the optic nerve ). He concepresd a new type and method of ecalauting glaucoma damage in people. All were awarded patents in US, Europe, and other countries. Dr. Solomon has 100 publications in various international journals.
Abstract:
Background: Semaphorin 3A is a leading factor in the apoptotic death program of the neural cells in CNS. It is right to suppose that inhibition of Sema3A expression in the right time window will reduce the death of a great population of neural cells following assault. Â Â Â
Purpose: To develop low molecular weight inhibitor of Sema3A and produce function blocking Sema3A human antibodies  Manufacture a biodegradable polymeric implant for controlled release of Sema3A inhibitor.        Â
Material and Methods: We used laboratory rats and rabbits and created acute and chronic assault to the optic nerve. Following the assault we injected the substances mentioned above in the injured eye. Â
Results: We present the methods of creating the low MW inhibitors of Sema3A and the Sema3A antibodies. The creation of the implants is shown. We present here the positive inhibitory activity of these substances in vitro and in vivo experiments.Â
Anita N Datta
University of British Columbia, Canada
Title: The use of mTOR inhibitor for the treatment of refractory seizures in an infant with hemimegencephaly

Biography:
Anita Datta is a Clinical Assistant Professor in Pediatrics at the University of British Columbia. She is a Fellow of the Royal College of Physicians and Surgeons of Canada, and is Board Certified by the American Board of Psychiatry and Neurology Child Neurology and Clinical Neurophysiology. She obtained her MD from the University of Saskatchewan, and completed Pediatric Neurology residency at the University of Alberta. She completed an Epilepsy and Clinical Neurophysiology fellowship at Boston Children’s Hospital. She is a national examiner for the Canadian Society of Clinical Neurophysiology. She is currently program director of the epilepsy fellowship training program. Her primary clinical interest is epilepsy and its surgical management. She is also involved in the Tuberous Sclerosis Clinic and is part of the Ketogenic Diet team. Her research interests include clinical epilepsy, neurophysiology and neuropsychological outcomes. She has authored peer reviewed publications and book chapters in these areas.
Abstract:
Hemimegalencephaly (HME) is a hamartomatous malformation involving one cerebral hemisphere, often resulting in treatment resistant seizures, intellectual disability, and autistic features. Hemispherectomy is the definitive treatment, but there is risk of high morbidity and mortality, especially when done in early infancy. Various preclinical studies have shown that dysregulation of the mTOR pathway has an integral role in the development of various epilepsy syndromes, including tuberous sclerosis complex (TSC), focal cortical dysplasia and HME. Recently, mTOR inhibitors were proven to effective in treating seizures in TSC. We present a case of a patient, who presented at 6 days of age with treatment resistant epilepsy, despite the trial of 9 anti-seizure medications and the ketogenic diet. As the patient was awaiting epilepsy surgery, an mTOR inhibitor, rapamycin was initiated. After 1 week of the initiation, she had more than 50% reduction in seizure frequency and total seizure burden and the duration of seizures decreased. (Total seizure burden was calculated as the total amount of time occupied by electrographic seizures during the video-EEG monitoring.) At two weeks, the parents felt that for the first time, she was making developmental gains. She also appeared brighter and more interactive. Due to her response to treatment, her hemispherectomy was deferred to when she was older with an increased weight. She had a functional hemispherectomy without any complications and is now seizure free. This case exemplifies how mTOR inhibitors should be considered as a treatment option for patients with HME and refractory epilepsy.
Young-Ho Lee
Hanyang University College of Medicine, South Korea
Title: Delayed cytokine effects of 4 days of intravenous G-CSF infusion for mobilization of peripheral blood stem cells: Possible role for neuroregeneration

Biography:
Lee is a professor of department of pediatrics, Hanyang University Medical Center. He earned his degree of M.D. and PhD at Hanyang University College of Medicine. He got postgraduate researcher course in the field of pediatric hematology and stem cell transplantation at the UCLA Medical Center. His major fields are pediatric hematology, hematopoietic stem cell transplantation, and stem cell biology including stem cell homing. He performed the first successful cord blood transplantation (CBT) for child with relapsed acute leukemia at 1998 in Korea. Since then, he established infrastructures of CBT regarding banking guidelines for CB as well as clinical guideline for CBT. Furthermore, he performed the pioneering works for legislation for CB act in Korea. Recently, he has tried the application of mononuclear cells of CB and mobilized peripheral blood stem cells as cell therapeutics for refractory neurologic diseases.
Abstract:
Statement of the Problem: Granulocyte colony-stimulating factor (G-CSF) has been widely used to mobilize peripheral blood stem cells (PBSC). In addition, it also has been tried to reveal the regenerative potential in various neurodegenerative diseases. We investigated the short-term and delayed effects of infused G-CSF for PBSC mobilization on the various cytokine secretions in cerebral palsy (CP) children. Methodology & Theoretical Orientation: G-CSF (10μg/kg/dose) was administered subcutaneously for 4 days to the children with CP. In first group, blood levels of G-CSF, interleukin (IL)-6, IL-10, insulin-like growth factor (IGF-1), vascular endothelial growth factor (VEGF), and brain derived neurotrophic factor (BDNF) as well as mobilized total nucleated cell (TNC)/CD34+ cell counts in peripheral blood (PB) were compared between levels just before (D+0) and 1 day after 4 days of G-CSF injections (D+5). In second group, cytokine levels were compared between D+0 and 1 month after 4 days of G-CSF injection (D+30). Cytokine levels were measured by enzyme-linked immunosorbent assay. Findings: Baseline levels of G-CSF were significantly increased (p=0.000) and IGF-1 decreased (p=0.011) at D+5 after 4 days of G-CSF compared to control group. In contrast, other cytokine levels including IL-6, IL-10, VEGF, and BDNF did not show any significant changes between before and after G-CSF administration. CD34+ cell counts (p=0.000) as well as TNC counts (p=0.000) in PB were significantly increased from D+0 to D+5 in children who received G-CSF compared to placebo group. Regarding delayed effect of G-CSF, G-CSF levels were significantly increased from baseline to D+30 (p=0.000), along with the increase IL-10 (p=0.035) and VEGF levels (p=0.011) and the decrease of IGF-1 levels (p=0.014). Conclusion & Significance: G-CSF which administered to mobilize PBSCs could induce the delayed effects on the levels of G-CSF itself as well as of other cytokines which could affect on the neuroregenerative potential.
Hyo Joon Kim
Presbyterian Medical Center, Korea
Title: The effects of combination treatment with PME-88 & Riluzole on the ALS Mouse model

Biography:
Born in South Korea. Kim studied Medicine in Kyoungpook National University and trained Neurosurgery in Presbyterian Medical Center. Kim’s research is based on neuroscience study group, Honam Stroke Research Group. Kim’s major research subject is increasing disrupted brain function in stroke, traumatic brain injury and ALS disease. Related with ALS, Kim’s study started with electrical stimulation on the cortical motor cortex area and tried to extent pharmacological treatment combination.
Abstract:
Amyotrophic Lateral Sclerosis, or ALS, is a critical degenerative neurological disorder caused by the progressive destruction of motor neurons. Approximately 20% of all familial cases of ALS result from a genetic defect on chromosome 21, leading to mutation of the superoxide dismutase 1 (SOD1) enzyme. In this study, we investigated different treatments for ALS on the ALS mouse model and found that the treatment using the combination of PME-88 and Riluzole through oral administration produces a greater effect than the treatment using only Riluzole, which is the only method approved by the FDA. The ALS mouse model was divided into three groups; a PME-88 group that would ingest PME-88(n = 8 animals/group), a Riluzole group that would ingest Riluzole(n = 11 animals/group), and a combination group that would ingest both PME-88 and Riluzole(n = 11 animals/group). We observed and evaluated the effects of the three different treatments on the functional maintenance of motor neurons. Results showed that the combined treatment of Riluzole and PME-88 is most effective in maintain the motor function of motor neurons. We also found that symptoms of ALS appeared at the latest in the combined-treatment group than in the other two groups. However, the differences in the amount of time survived between the three groups were insignificant. In conclusion, we found that combined treatment showed the greatest positive effect on the maintenance of the motor function in the ALS mouse model. We had hypothesized that SOD, the source of PME-88, would increase the treating effect of Riluzole
Kay Chang
University of Macau, People’s Republic of China
Title: Exploring the Cultural-Specific Challenges and Opportunities of the Autism Spectrum Disorders Populations in China and Hong Kong

Biography:
Kay CHANG (Kay Sio-Ngã Chang, Psy.D.), is an Assistant Professor of psychology at the University of Macau. She actively applies the scientist–practitioner framework in both her academic and clinical work since her graduation from the California School of Professional Psychology, Alameda. She is an US licensed clinical psychologist and an UK chartered clinical psychologist who has a noticeably diverse experience base by having practiced in US, China, Hong Kong and Macau. She also volunteers for going consultations in abuse cases and disaster trauma work. Her research interests include the applied aspects of positive psychology, medical anthropology, professional development issues, addictive behaviors, creativity factors and resilient capacities.
Abstract:
There is a wealth of evidence detailing the efficacy of interventions in the treatment of Autism Spectrum Disorders. However, the existing research knowledge base on the use of this intervention in this population in regions outside of the United States and Europe is far more modest. In particular, there is limited data on the efficacy of Applied Behavior Analysis in the treatment of individuals with Autism Spectrum Disorders residing in regions of greater China (e.g., the People’s Republic of China, Hong Kong). To understand the treatment challenges faced by the families and service advocates for this clinical population, a review of treatment-based research studies and local community service providers were included to explore the possible cultural-specific challenges despite the diagnostic and neuropharmacological advances. Opportunities of effective pharmacological and behavioral strategies for the Autism Spectrum Disorder populations in China and Hong Kong is explored.

Biography:
Dr. Shen Jiangang is Professor in School of Chinese Medicine, University of Hong Kong. He also serves as Associate Director (Research) and Chair of Department of Research Postgraduate Students Committee in the School. Dr. Shen’s major research interests focus on molecular regulations of oxidative stress and redox signaling in brain damage and brain repair in post-stroke and neurodegenerative diseases. He is also interested in the experimental and clinical studies on Chinese herbal medicine for cerebral and cardiovascular diseases. His studies have been supported by many prestigious research funds from Hong Kong, Mainland China and others. He has published more than 150 peer-reviewed papers in prestigious academic journals and 14 book chapters. He received many academic and research awards and appointed as honor professorship 15 universities from China and USA. He serves as the editorial board members for many international academic journals including Toxicology and Applied Pharmacology, Scientific Reports and others.
Abstract:
AIM: Tissue plasminogen activator (t-PA) is the only FDA approved drug for acute ischemic stroke, but its use is limited with the therapeutic time window within 4.5 hours and hemorrhagic transformation (HT). We aim to test the hypothesis that peroxynitrite (ONOO-), a representative of reactive nitrogen species, could be a critical therapeutic target for preventing delayed thrombolytic HT and improving outcome in ischemic stroke. We tested whether peroxynitrite decomposition catalyst (PDC) could prevent such complication. Furthermore, we investigated that baicalin, a natural antioxidant, could scavenge ONOO- and prevent HT in ischemic stroke animal model with delayed t-PA treatment.
METHODS: Male Sprague-Dawley (SD) rats were subjected to middle cerebral artery occlusion (MCAO) with t-PA (10 mg/kg) or t-PA plus FeTMPyP (3 mg/kg, a representative PDC) or baicalin (10, 25, 50 mg/kg) at MCAO for 2 or 5 h and reperfusion for 22 or 19 h, respectively. HT was assessed with hemoglobin assay. Neurological deficit was evaluated with Modified Neurological Severity Score (mNSS). Peroxynitrite was examined by detecting 3-nitrotyrosine (3-NT) and our newly developed high selective ONOO- fluorescent probe. The expression and activity of MMP-9/MMP-2 were assessed by western blotting and gelatin zymography.
RESULTS: T-PA infusion at 2 h after cerebral ischemia did not induce HT but attenuated neurological deficit, whereas at 5 h significantly induced HT and worsened neurological outcome. Co-treatment of FeTMPyP revealed to prevent HT and improve neurological functions. Early t-PA infusion at 2 h inhibited iNOS activity, ONOO-production, MMP-9/MMP-2 expression and activity, whereas delayed t-PA infusion at 5 h up-regulated iNOS activity, increased 3-NT formation, and down-regulated MMP-9/MMP-2 expression and activity. Co-treatment of FeTMPyP revised those changes in the ischemic brain with delayed t-PA infusion 5 h. Meanwhile, Baicalin revealed strong ONOO--scavenging activity and protected the neuronal cells from ONOO--induced neurotoxicity, reduced infarct size and attenuated apoptotic cell death and HT.
CONCLUSION: Peroxynitrite could be a critical therapeutic target for preventing hemorrhagic transformation and improving neurological outcome in ischemic brains with delayed t-PA treatment.
Hala Fakhiry
Cairo University, Egypt
Title: Emotional empathy and cognitive styles in psychodynamic group therapy: UAE experience

Biography:
Hala Fakhiry is a Professor of Psychiatry in Cairo University, Egypt. She is also the Head of Psychiatric Department at Kuwaiti Hospital, Sharjah, UAE. She is a member of APA, CCPA, CACCF, EPA, and EGTA with Clinical Experiences for 29 years in management of Psychiatric cases, Liaison Psychiatry and Addiction treatment. She is Skilled in psychotherapy (Psychodynamic) and has Medico Legal & Forensic Psychiatry Experiences. She is sharing in Psychiatric National and International Conferences across the Globe (1998-2017).Dr Hala has over than 30 publications in both National and International Journals (1993-2017) and Teaching Experiences for undergraduate and postgraduate students.
Abstract:
Background: Practice of group therapy has been unexpectedly accepted against the pre-assumption that patients could reject the idea of self-disclosure in presence of strangers.
Objectives: The present study is designed to study group psychotherapy experience in United Arab Emirates (UAE). The group cohesion process along the time of therapy is studied. A trial is also made to explore impact of attending these types of groups on aspects of thinking described as cognitive styles as fears of failure and anger expression; as well as cognitive orientation of emotions and empathy.
Method: In the current case- control study 80 patients (40 males and 40 females) between 19 – 45 years old with different DSM-IV psychiatric diagnoses were recruited and subdivided into four groups. Each group contained 20 patients; 20 males and 20 females allocated to attend group therapy (Male Group (MGp) & Female Group (FGp), while other 20 males and 20 females allocated as comparative groups not attending group therapy (Male Comparative (MCm) & Female Comparative (FCm). All groups were further compared with frequency matched healthy volunteers served as control group that consisted of (20) males in MCl group and (20) females in FCl group. Sharing groups were subjected to clinical psychiatric examination and base line psychometric assessment using Fear Of Failure (FOF1), Trait Meta Mood Scale (TMMS1), Arabic Anger Scale (AAS1) and Emotional Empathy scale (EES1). Each patient in Male Group (MGp) & Female Group (FGp) attended at least 40 sessions in closed group along 1year duration. Group cohesion was monthly assessed using GCS (1-12) for both groups. Psychometric re-evaluation at the end of 1year was made for all groups using same tests (FOF2), (TMMS2), (AAS2) and (EES2). All available scores were subjected to statistical analysis.
Results: Base line readings showed statistically significant higher scores of (FOF1) and (AAS1) in patients groups compared to control groups (p< 0.00001) and lower scores of TMMS1 and EES1 (P=0.0020 for the 3 male groups & P<0.00001 for the three female groups). However, differences between groups of patients (MGp vs. MCm) and (FGp vs. FCm) were non-significant in FOF1 (p=1 & p=0.28809), AAS1 (p=1 & p=0.5186), TMMS1 (p=0.6326 & p=0.6773)& EES1 (p=0.7491 & p=1). Generally females showed more regular attendance of group sessions compared to males but difference was non–significant statistically. Patients’ assessment of group cohesion generally increased along the 12 months as denoted by GCS scores. Patients attending group therapy demonstrated variable levels of improvements compared to other groups of patients not attending group therapy and compared to controls. FOF2 demonstrated definite improvement in MGp compared to MCm group (p=0.0283) and in FGp compared to FCm group (p=0.0480) but still improvement is beyond normality compared to control groups (p< 0.00001). EES2 demonstrated definite improvement in MGp compared to MCm group (p=0.01813) and in FGp compared to FCm
group (p=0.038434) and improvement could reach normality level compared to control groups (p non-significant). All TMMS2 scores of patients groups increased on treatment regardless attending group therapy or not. Improvement in males reached normal levels compared to control group (p=0.1220 for the 3 male groups); but not for female patients (p= 0.0021 for FGp vs. FCl). However, FGp patients showed more improvement than FCm group (p=0.0044). AAS2 demonstrated definite improvement in scores of all groups of patients after treatment with no significant difference between MGp&MCm group (p=0.6756) or FGp&FCm group (p=0.1903) but still improvement is beyond normality by comparison with control groups (p< 0.00001).
Conclusion: Group therapy has been successfully accepted among UAE psychiatric patients improving their fears about failure and empathy and to variable degree cognitive orientation of emotions but not anger expression.

Biography:
Yeonseung Han is improving his expertise and passion in Yonsei university, college of medicine. His experience of research forum was started from Gwangju-science high school. He studied about Korean traditional preserving method; blackening wood surface of furniture or structure. Then he did oral presentation in 2011-year-held CASTIC as a Korean representative with this research. He studied biological science in KAIST(Korean advanded institute of science and technology) and KIT(Karlsruhe institute of technology) as a exchange student. To study and do research on human disease in particularly brain field, he is studying on ischemic stroke part in Yonsei university.
Abstract:
The inflammatory response following acute ischemic stroke is a well-known and widely studied phenomenon. However, the mechanism of neuro-inflammation is still unknown. Microglia and monocyte are now recognized to play a major role in neuro-inflammation after ischemic stroke. Microglia are the resident macrophages of brain. Macrophages originated from monocyte also have a highly phagocytic capacity after ischemic stroke. In this study, we explored the activated microglia by ischemic stroke affect to differentiation of monocyte. BV-2 cells (microglia cell line) were treated with lipopolysaccharides (LPS; 10ng/mL) for polarization to M1 phenotype and treated with interleukin-4 (IL-4; 20ng/mL) for polarization to M2 phenotype. After BV2 cells were activated with LPS and IL-4 for 1 d, cells were washed and M1 and M2 phenotype conditioned media were harvested at 3 d. THP-1 cells (monocyte cell line) were cultured in M1 and M2 phenotype conditioned media of BV2 cells. THP-1 cells were also treated with each following substances; IL-10, IL-1 beta, TGF-alpha and TGF-beta. It is well known that CD11b positive cells consider as M0 macrophage, CD86 positive cells as M1 macrophage and CD206 positive cells as M2 macrophage. THP-1 cells treated with M2 phenotype conditioned media expressed CD206 immunoreactivity in condition with and without phorbol-12-myristate-13-acetate (PMA; 10ng/mL). And, CD11b immunopositive cells were significantly high in the IL-1 beta and TGF-beta treated group. CD206 positive cells were also highly observed in the TGF-beta treated group but less than M2 phenotype conditioned media treated group. Our data supports that the cytokine secreted from M2 phenotype microglia might induce differentiation of monocyte into M2 phenotype macrophage in in vitro system.
Zeynab-Sadat Payambarpour
Shahed University, Iran
Title: The antiangiogenic activities of Synanthedon tipuliformis sexual pheromone on chorioallantoic membrane

Biography:
Zeynab-Sadat Payambarpour got her Master’s in Linguistics and then considering the interdisciplinary fields she chose Cognitive Sciences for PhD but facing some of the biological courses she preferred to get another Master’s in Physiology and then with deeper knowledge wants to pursue PhD. She is now a Postgraduate Student of Physiology in Tehran Shahed University. She and her professor Dr. Majid Hassanpour-Ezatti have been working on neuroscientific projects and the effects of some pheromones on angiogenesis. She has been teaching and working over 10 years now and enthusiastically pursuing academic studies and research.
Abstract:
Many chemicals or substances might be associated with inflammation-induced angiogenesis which have not been discovered yet. So far we know some of the pheromones can reduce inflammation. Currant borer, Synanthedon tipuliformis, (Sesiidae); leopard moth, Zeuzera pyrina L. and pistachio twig borer, Kermania pistaciella (Lepidoptera: Oinophilidae) are three pest insects with well-known sex pheromones whose main active components of their sex pheromones are E2,Z13-18:OAc; (E, Z)-2, 13-octadecadien-1-ol acetate and (2S,12Z)-2-acetoxy-12-heptadecene, respectively, together with a series of lipid derivatives. We hypothesized that these pheromones may contain angiogenesis modulators. In the current study, we investigated the effects of the pheromones alone or in combination with paclitaxel on angiogenesis in chorioallantoic membrane. These pheromones demonstrated potent in vivo anti-angiogenic activity, which exceeded that of their solvents as reference agents. All tested pheromones showed the most potent anti-angiogenic activity, which was twice that of their solvents, as well combination of all of them with paclitaxel induced the most potent anti-angiogenic effect. This highlights the importance of identifying pro- and anti-angiogenic property in these pheromones not only for the development of novel angiogenesis modulators for the treatment of diseases such as cancer, but also their use as adjuvants for chemotherapy agents.
Kadhim Alabady
Public Health and Safety Department - Dubai Health Authority (DHA), UAE
Title: Mental Health challenges among women in Dubai, What Commitments are needed? Public Health and Safety Department - Dubai Health Authority (DHA)

Biography:
Hold a Doctorate degree in Public Health and Epidemiology, Master degree in Clinical Epidemiology (MSc), Master degree in Public Health (MPH), all from The Netherlands Universities.
· Worked in Public Health since 1999 at different levels such as:
- Academic (Erasmus university – Rotterdam / The Netherlands, Queen Marry University – London / UK), University of East Anglia UEA / Norwich.
- International (United Nations).
- National Health Authority (Qatar).
- National Health Service (NHS), UK since Feb 2007.
- others
· Registered as Epidemiologist Grade A with The Netherlands Epidemiological Society.
· Has numerous publications in the UK in mental illnesses, cancer, cardiovascular diseases, diabetes, Dementia, Autism, COPD, population health, road casualties and others.
·Has broad experience with a wide variety of statistical software programs i.e. SPSS, STATA, excel, etc.
· Broad experience of R&D.
· Designing, conducting, analysing, and presenting quantitative and qualitative researches.
Abstract:
Purpose: Mental health problems affect women and men equally, but some are more common among women. To Provide a baseline of the current picture of major mental health challenges among women in Dubai. which can then be used to measure the impact of interventions or service development.
Method: We have used mixed methods evaluation approaches. This was used to increase validity of findings by using a variety of data collection techniques. We have integrated qualitative and quantitative methods in this piece of work. Conducting the two approaches is to explore issues that might not be highlighted enough through one method.
Results: The key findings are:
·The prevalence of people who suffer from different types of mental disorders remains largely unknown, many women are unwilling to seek professional help because of lack of awareness or the stigma attached to it.
·It is estimated there were around 2,928–4,392 mothers in Dubai (2014) suffering from postnatal depression of which 858–1,287, early intervention can be effective.
·The system for managing health care for women with mental illness is fragmented and contains gaps and duplications.
· It is estimated 1,029 girl aged 13–19 years affected with anorexia nervosa and there would be an estimated 1,029 girl aged 13–19 years affected with anorexia nervosa.
Recommendations:
•Work is required with primary health care in order to identify women with undiagnosed mental illnesses. Further work is undertaken within primary health care to assess disease registries with the aim of helping GP practices to improve their disease registers.
•It is important to conduct local psychiatric morbidity surveys in Dubai to obtain data and assess the prevalence of essential mental health symptoms and conditions that are not routinely collected to get a clear sense of what is needed and to assist decision and policy making in getting a complete picture on what services are required.
•Emergency Mental Health Care – there is a need for a crisis response team to respond to emergencies in the community.
•Continuum of care – a significant gap in the services for women once they diagnosed with mental disorder.
Sigal Fleisher-Berkovich
Ben-Gurion University of the Negev, Israel
Title: Modulation of glial activation and amyloid burden by telmisartan: in vitro and in vivo studies

Biography:
Sigal Fleisher-Berkovich has completed her PhD at the age of 29 years from Ben-Gurion University of the Negev. She is an associate professor in the department of Clinical Biochemistry and Pharmacology. She has published papers and book chapters in reputed journals and serves as a reviewer of repute journals. She also received highly competitive national and international grants.
Abstract:
The circulating renin-angiotensin system (RAS) is a fundamental regulatory mechanism of blood pressure conserved through evolution. Apart from periphery, an intrinsic RAS was also identified in the brain in which the bioactive hormone, angiotensin II, plays multiple roles. Angiotensin II (Ang II), is formed from angiotensin I by angiotensin converting enzyme (ACE). It acts mainly through angiotensin type 1 receptors (AT1Rs) and can influence brain inflammation expressed in Alzheimer’s disease (AD) models. Although increased levels of brain AT1Rs, Ang II and ACE were reported in AD models, the role of RAS in brain inflammation remains unclear. Telmisartan, a well-known anti-hypertensive drug and an AT1R blocker, was suggested to serve as a potential treatment for brain inflammation and AD. The present study shows that intranasally given telmisartan (1mg/kg/day) for 3.5 weeks to 2 month significantly reduced amyloid burden and microglial activation by up to 50% in the cortex of five familial AD (5XFAD) mice. Hippocampal amyloid plaques and microglial activation in 5XFAD were also reduced following 2 months treatment with telmisartan by approximately 50% and 25%, respectively. Short term effects of telmisartn in vivo were compared to those of perindopril (angiotensin converting enzyme inhibitor) which exhibited a similar inhibitory effect on the expression of these associated AD markers. In vitro studies including LPS-induced BV2 microglia cells treated with telmisartan resulted in a significant attenuation of inflammatory mediators' production including tumor necrosis factor-α (~ 50% reduction), interleukin 1-β (~30% reduction) and nitric oxide (~60% reduction). Telmisartan effect on NO production in LPS-induced BV2 cells was confirmed in primary neonatal rat microglial cells as well. In LPS-induced primary microglial cells telmisartan reduced the NO production levels by up to 70% and in mixed glial cells by 60 %. Our data may envision potential intervention with the progression of glial activation and AD with both telmisartan and perindopril. Moreover, the non-invasive intranasal delivery may serve as an efficient alternative for systemic administration to modulate the brain RAS.
Hamid Irannejad
Mazandaran University of Medical Sciences, Iran
Title: Neuroprotective activity of novel 5,6-Diaryl-1,2,4-triazine derivatives with ethyl acetate moiety against H2O2 and Aβ-induced neurotoxicity

Biography:
Hamid Irannejad has completed his Pharm.D at Kerman University of Medical Sciences and PhD at Tehran University of Medical Sciences, IRAN. Postdoctoral studies was accomplished at University of Siena, Italy, under the supervision of Prof. Maurizio Botta. Currently, he is serving as an assistant professor at Mazandaran University of Medical Sciences. He has published nearly 20 papers in reputed journals in the field of medicinal chemistry.
Abstract:
Alzheimer’s disease (AD) is a neuropathologic disorder characterized by intracellular neurofibrillary tangles and amyloid aggregates in the CNS. In recent years numerous approaches have been used to combat AD like small molecule inhibitors of Aβ aggregation, anti-inflammatory agents, cholinesterase, a- and β-secretase.
Herein, we report synthesis of some 5,6-diaryl-1,2,4-triazines 3a-f and 8a-e as potential agents for treatment of AD. We evaluated them against both H2O2 and β-amyloid induced toxicity in PC-12 and SH-SY5Y cells and the extent of cell viability and apoptosis were assessed during 24 and 48 h of treatment.
All compounds showed significant neuroprotective activity with EC50 values ranging from 14-30 µM. Most compounds could increase cell viability compared to amyloid treated group.
Surprisingly, 3-thioxo-1,2,4-triazin-2(3H)-yl)acetate derivative 8e was the most potent compound in both tests with EC50 of 14 µM in H2O2 induced apoptosis and could increase 40% of cell viability revealed by cytometric analysis with Annexin V/PI staining. It was also shown that 8e has more neuroprotective activity than Quercetin in beta-amyloid induced toxicity. Moreover, compound 8e attenuated late-apoptosis from 42% to 6% (P<0.005) and 7% to 1% at 24 and 48 hour respectively compared to amyloid treated cells. Similarly, apoptosis was reduced from 12% to 4% at 24 hours. LDH release was not changed at any time points, pointing anti-apoptotic effect of compound 8e. Morphologic evaluation of cells by DAPI staining and TUNEL assay showed the effectiveness of this compound to improve neurite outgrowth and to prevent apoptosis and DNA fragmentation in neuronal cells.
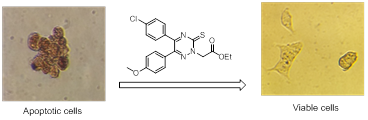

Biography:
Abstract:
Introduction: Five million people worldwide have epilepsy and 3 million of them are children. Phenobarbital is one of the oldest, safest and most available anti-epileptic drugs. The drug approved by WHO as first-line therapy for partial and generalized tonic-clonic seizures. Behavioral problems including hyperactivity, aggression, inattention and restlessness are seen due to phenobarbital. Therefore, we evaluate the effectiveness of vitamin B6 on behavioral disorders due to phenobarbital in epileptic patients.
Methods: In this study, 77 patients with seizures between 2 and 15 years were enrolled in two groups .One group received Phenobarbital plus vitamin B6 and the other group Phenobarbital plus placebo .After 3 month we change two groups and crossed them (after 10 days washed out period)and study continued for 3 month again. Behavioral parameter are evaluated in starting of study ,3 month later and at the end of study(6month later) using the Modified " Conner’s" questionnaire and the data were collected and analyzed by statistical software.
Results: There was no difference in hyperactivity, attention and aggression between two groups at the end of 3 month study but after crossing two groups we found statistical difference between two groups in hyperactivity (P value<0.01).This study showed that behavioral disorders due to Phenobarbital use in epileptic children reduced overtime and if we prescribe Vitamin B6 with phenobarbital this improvement will be more significant.
Conclusion: This study showed that behavioral disorders due to Phenobarbital use in epileptic children reduced overtime and if we prescribe Vitamin B6 with phenobarbital this improvement will be more significant



























